Continence Pads and Perineal Care
In this Health Topic
Urinary incontinence, or the involuntary leakage of urine, is a common condition affecting 1 in 3 women. Many people experiencing incontinence fail to seek help. There are different types of incontinence and many causes. With the correct assessment and treatment plan, incontinence can be cured or significantly reduced. Therefore, it is strongly recommended to seek help. When continence cannot be fully achieved, or the woman chooses to forego medical or surgical treatment, the use of continence pads is an option.
There are many brands of continence pads available. Pads can be purchased at supermarkets, chemists/drug stores, and online outlets. Some healthcare providers may also offer a continence service that provides continence pads.
There are two main types of continence pads: washable fabric pads and disposable pads. Fabric continence pads may either be built into pants/briefs (Figure 1) or be inserted into pants/briefs. Those built into pants/briefs come in a variety of sizes based on hip and waist measurements. Fabric pads are washable and suitable for light to moderate urinary incontinence.

Figure 1
Disposable pads (Figures 2a and 2b) can accommodate varying capacities as well as different levels of ability/agility.

Figure 2a

Figure 2b
Disposable pads consist of several different layers (Figure 3). There is a plastic, breathable backing sheet, and a one-way cover sheet that sits next to the skin and allows the urine to flow into the pad but prevents it from seeping back out. Pulp, like cotton wool, is sandwiched between these two layers. The pulp layer contains strategically placed super absorbent polymers to offer greater absorbency where it is needed. The polymers lock the urine away.
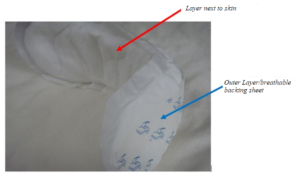
Figure 3
Those who suffer from incontinence may be tempted to wear sanitary napkins to contain their incontinence. This tends to be unsuccessful, since sanitary napkins are designed to absorb and contain blood rather than urine, which is more liquid. Some people use more than one sanitary pad at a time to combat the overflow. This is also not advisable. Dedicated continence pads are a more suitable option.
Pad manufacturers offer an extensive range of products with varying capacity from light incontinence to very heavy incontinence. When selecting the capacity of the pad, consider the amount and types of fluid you take in, how frequently incontinence episodes are occurring, and when possible estimate how much urine is being leaked at a time. Generally, there is no need to change the pad each time an incontinence episode occurs. Most products will have a wetness indicator which will identify when the pad requires changing. It is not recommended to change pads with superabsorbent polymers too frequently, as the polymers will absorb moisture and dry out the skin.
Disposable pads come in varying shapes and sizes. The higher the absorbency of a pad the bigger the pad will be. Insert pads are meant to be worn in conventional pants/briefs or special stretch/net pants (this is often referred to as a 2-piece system). The aim is for the pads to be fitted and held snugly against the genital area to prevent leakage. Each manufacturer will have their own specific guidance for application of these pads. If using stretch pants, accurate measurement of the hips and waist is required. Leakage occurs when there is not a good, snug fit.
Pull-up pads are also available and give a sense of wearing one’s own underwear/pants (Figure 4). These come in varying sizes and capacities and also require accurate hip and waist measurements to ensure a proper fit. Pull-up pants tend to not be as absorbent as the larger 2-piece systems.

Figure 4
For individuals who have disabilities, there are all-in-one pads and belted pads. The belted pads facilitate toileting for people who require hoisting for toileting. These vary in size and capacity, so hip and waist measurements will be needed to ensure a good fit.
If fabric pads are chosen, they need to be washed before use to activate them. DO NOT use fabric conditioner, as this waterproofs the pads and makes them ineffective.
It is recommended that continence pads be stored in a dry, ambient environment, and not removed from the packaging that they come in. Pads should be removed one at a time, as needed. Do not crush the pads, as this will break up the pulp and make them less effective.
Continence pads are available to accommodate varying capacities. While it is tempting to use the most absorbent pad to give a sense of security, this approach may not be best for maintaining the health of your skin.
There should be no odor when the pads are correctly applied and used. Odor occurs when the air mixes with urine. It is important to cleanse the skin when changing the pad. A ‘wash’ that has a pH of 4-6 is recommended to prevent the skin from becoming sore. Using baby wipes to cleanse the skin is not recommended, however, you can buy skin foams and wipes that are specially designed for patients who experience incontinence.
Maintaining a healthy, balanced diet will help keep the skin in optimum condition. Maintaining fluid intake of 20-30 ml/kg daily and avoiding caffeine and artificial sweeteners will help to prevent dehydration.
When using barrier creams, avoid oil-based creams as they can affect the absorption of the pads by blocking the cover sheet and leading to the skin becoming bathed in urine. If skin protection is required, films (which can be in the form of sprays, foams, or wipes) or barrier creams that dry into a film are recommended. Discuss with your healthcare professional where these can be obtained and the best ones to use. In general, barrier products should be applied sparingly, and the manufacturer’s guidance should be followed.
