Non-Surgical Approaches to Managing Bladder Problems
Introduction
Bladder problems are common, often causing distressing and inconvenient symptoms. Bladder problems can cause you to leak urine during activities, rush to the toilet many times during the day and night, and sometimes leak urine before you reach the toilet. This leaflet explains how physiotherapy addresses continence issues and bladder symptoms, looking at treatable physical aspects related to urinary incontinence and the use of conservative (non-surgical) measures to help manage bladder problems.
In this Health Topic
Stress urinary incontinence (SUI) is the involuntary leakage of urine on physical exertion, including sporting and working activities (running, walking), sneezing, coughing, laughing, lifting, bending, and moving from lying to sitting and sitting to standing. For more information on SUI, click here.
The pelvic floor muscles are supportive muscles attached to the walls of the pelvis. They stretch like a sling from your pubic bone at the front to the coccyx (tail bone) at the back. The pelvic floor muscles help support the internal organs and close the bladder outlet (urethra) and back passage (rectum), helping to prevent leakage. These muscles are also important for sexual activities, such as erection and ejaculation in men and guiding penetration of the penis during intercourse, enjoyment, and orgasm in women. For more information on pelvic floor exercises, click here.
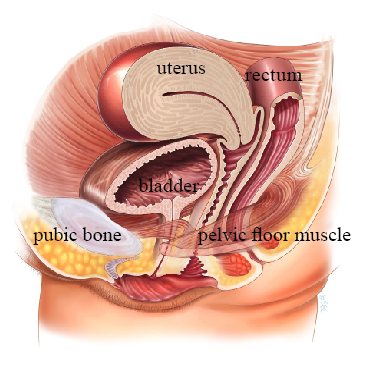
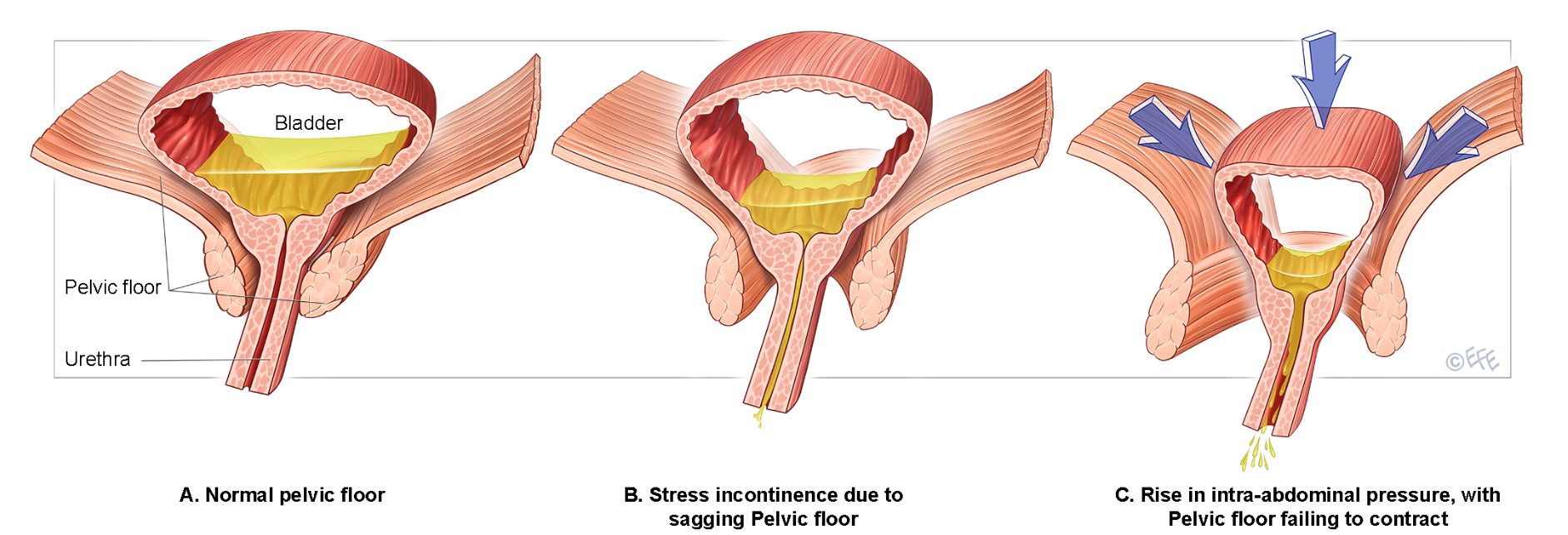
The urethral closure mechanism keeps you dry during an increase of intra-abdominal pressure. You can compare this mechanism with stopping the water stream of a hose. To stop the stream, you can squeeze the hose, or kink it, or put your foot on the hose after putting it on a firm surface. The same happens in the pelvic floor: the pelvic floor muscles can squeeze around the urethra (tube draining the bladder) and clamp the urethra between the pelvic floor muscles and the pubic bone, hence increasing the intra-urethral pressure and stopping the flow of urine.
Intra–abdominal pressure increases every time you cough, sneeze, or lift a heavy object. This increase of pressure should be transmitted equally to the bladder and the urethra. If the pelvic floor muscles are weak, they cannot increase the intra-urethral pressure enough to close off the urethra. This is when leakage occurs.
There is a complex interplay between the muscles, nerves, ligaments, and support around the urethra which are in turn affected by injury, hormones, aging, etc. Some examples of possible causes of SUI include:
- Weak pelvic floor muscles. These are the muscles that cover the base of the pelvis. Their main job is to hold the pelvic organs in place, to protect these organs, and to stop any undesired leakages of urine, feces, and gas. Furthermore, by adequately relaxing these muscles passing urine and stool is possible.
- Being overweight. Extra weight on the pelvis and the pelvic floor muscles, which leads to a continuous increase of intra-abdominal pressure, decreases the closure mechanism around the urethra, especially during any of the physical exertion activities previously listed.
- Pregnancy and childbirth. Approximately 1 in 3 pregnant women suffer from SUI. Extra weight gain, hormones, and changes in muscle balance around the pelvis all contribute to the risk of developing continence problems. Childbirth can also result in trauma to the vaginal walls, pelvic floor muscles, nerves and local ligaments, which can decrease the overall continence support of the pelvic area. If there is urine leakage immediately after childbirth, allowing time for the pelvis to heal may result in a decrease in SUI.
- Persistent cough. Every time you cough, you increase the pressure in your abdomen, which in turn presses down on the bladder. This can force the bladder to expel a bit of urine. If you suffer from a chronic cough, this process will happen frequently.
- Chronic constipation. Repetitive straining during bowel motions puts pressure on the pelvic organs and the pelvic floor muscles, thereby weakening them and increasing the risk of bladder descent and incontinence (as well as prolapse of other pelvic organs).
- Menopause and aging. Loss of estrogen at menopause and general aging may weaken the pelvic floor muscles, tissues, and ligaments and consequently decrease the support of the urethra, thereby contributing to urine leakage.
A physiotherapist can teach you how to use your pelvic floor muscles effectively and how to regain your former activities without leakage. Training the pelvic floor muscles strengthens them so that they can once again provide adequate support to your bladder and urethra. You will also learn how to time adequate contraction of these muscles, providing better automatic closure of the urethra against leaks when needed.
Your pelvic floor muscles act as a guard and maintain a gentle background tone. When you cough or sneeze, the muscles contract to provide support and to maintain sufficient closure of the urethra. Usually you are not even aware of this happening as it is mostly a reflex muscle contraction. In the beginning of your pelvic floor muscle training the physiotherapist will teach you how to consciously contract your pelvic floor muscles before you cough or sneeze. This strategy immediately helps to avoid involuntary leakages and usually works very well. Later on, physiotherapy aims to restore your normal automatic pelvic floor muscle contractions needed to avoid involuntary leakages during daily activities.
The physiotherapist not only treats your pelvic floor muscles, but also helps you to regain continence during your daily activities and gives you advice about how to adapt, modify, or change your lifestyle and behavior, fluid intake, medication and home training.
Urgency urinary incontinence (UUI) is the involuntary leakage of urine associated with a sudden, (nearly) irresistible need to pass urine. You may not make it to the toilet in time and leak.
Normal bladder capacity in adults ranges between 400-600ml. We usually experience the first bladder sensation when the bladder is approximately 150-200mls full. If you are anxious or stressed, this sensation is heightened. The first sensation then becomes a “need to go” feeling, which acts as a prompt to pass urine, usually before the bladder is actually full. Sometimes triggers, such as the sound of running water, cold weather, putting a key in the front door, or seeing a toilet, can cause the bladder to involuntarily contract, which may result in leakage before reaching the toilet. A vicious cycle may develop whereby you allow yourself to go often because you feel the urgency and you are worried about leaking. Over time, the bladder gets used to storing only small amounts of urine and is therefore not allowed to stretch properly, thus making you go to the toilet more frequently. This condition also makes some women wake up more than once at night to go to the toilet to pass urine, then go back to bed to sleep again. This is called nocturia.
There are many different underlying causes of which many are not clear yet, but UUI could be a symptom of overactive bladder (OAB). However, sometimes there is no apparent cause for UUI. For more information on OAB, click here.
Other causes of UUI are urinary tract infections, constipation, medication side effects, pelvic growths or swellings, and conditions affecting the nervous system such as multiple sclerosis and stroke. Proper assessment by your doctor will rule out any of these causes. It is also important to avoid any irritants to the bladder such as fizzy drinks, artificially sweetened drinks, caffeine, and alcohol.
Physiotherapy can help treat UUI through pelvic floor muscle contraction aimed at inhibiting the bladder muscle contraction, bladder retraining, fluids advice, medication advice, and behavioral modifications.
Following are some techniques to help you control your bladder more effectively:
- When you feel the urge to urinate, try to hold on.
- Keep calm and don’t panic.
- Stand still or sit down.
- Contract your pelvic floor muscles. This does not need to be a firm contraction but try to hold a moderate but continuous pelvic floor muscle contraction for about 30 seconds for 3 times, with 30 seconds of rest between these contractions. This may decrease the urgency.
- Stand on your tip toes or curl down your toes.
- Cross your legs.
- Press or rub on the backs of your thighs.
- Press an inch above the inside ankle bone.
- Gently press over the urethra in an upward direction.
- Try to distract your thoughts by focusing your mind on something else.
- Wait until the urgency passes, up to 30 seconds, then carry on with your activity or go to the toilet if appropriate.
- You may need to repeat some of these tips on the way to the bathroom such as walking there on your tip toes.
- Aim to drink 3-4 pints/1.5-2 liters/6-8 glasses of fluid every day.
- Eliminate/reduce caffeine intake. Green tea and hot chocolate both contain caffeine.
- Keep decaffeinated drinks to a minimum as they have been chemically altered to reduce the amount of caffeine and may irritate the bladder.
- Reduce your intake of alcohol and fizzy drinks, which can affect urgency and UUI as well as acidic foods such as citrus and tomatoes which may cause bladder irritation.
Bladder training may help your bladder to hold more urine. Ideally, you should have approximately 3-hour gaps between emptying your bladder. This is the goal, but you may need to start with shorter intervals and gradually increase the time between each void until this goal is reached. This may take several weeks and may be affected by the volume and type of fluid consumed. If you tend to get up in the night to empty your bladder, don’t drink for at least 2-2.5 hours before bedtime, and make sure your last drink is not fizzy, alcoholic, or caffeinated. If you do wake at night, don’t automatically get up. Try to ignore it and use some of the tips listed above. For more information on bladder training, click here.
There are a variety of different medications that can help with urgency and UUI. Besides taking any prescribed medication, it is still important to control what you are drinking and to try to train your bladder. The medications are designed to enable you to hold on for longer, reduce how often you need to go to the toilet (both during the day and night), and to reduce leakage. The medications do cause side effects such as dry mouth and constipation in some people. Sometimes you may need to try several different drugs before you find one that suits you. Constipation can be treated both by diet and medically, so you can still enjoy the good effects of the medication. Sometimes your bladder may improve after a few months of treatment, enabling you to come off the medication. However, many women do have to stay on the medication for a longer term in order to control their symptoms. Combinations of medications and physiotherapy have been proven to be better than either one alone.
Mixed urinary incontinence is a combination of both SUI and UUI. Many women have both types of incontinence and both may be managed with a number of the conservative measures listed above.
Incomplete bladder emptying is a bothersome symptom where some women experience the sensation of not having emptied their bladder properly or get some urinary dribble or leakage after the main volume of urine has passed. This is a common complaint in women who have vaginal prolapse, in particular the front wall of the vagina. For more information on pelvic organ prolapse, click here.
Following are some techniques to help you empty your bladder more effectively:
- Always sit on the toilet with your feet and knees apart and your feet on the floor. Never crouch or hover over the toilet seat, as this does not allow your bladder to empty fully.
- Bend forward from your hips and rest your forearms or your hands on your knees.
- Keep the normal curve in your back and relax your abdominal muscles.
- Relax and take your time.

After passing urine:
- Sit up, then lean forward again. Relax and wait to see if any more urine comes out.
- Stand up, wriggle, then sit down again. Lean forward and relax.
- Tilt the pelvis forward and backward while sitting on the toilet.
- Tap, spring or press the bladder, then lean forward and relax again.
- Some women find it necessary to push their prolapse back in order to properly empty the bladder. This is known as “splinting.”
- When you think you have finished, gently contract the pelvic floor muscles, hold for a few seconds, and then relax.
