Pelvic Floor Exercises
In this Health Topic
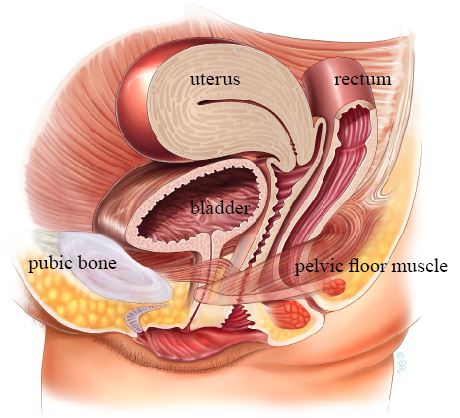
The pelvic floor is composed of a thin sheet of muscle fibers and associated connective tissue which spans the area underneath the pelvis between the pubic bone at the front and the sacrum or tail bone at the back (see illustration below).
- The pelvic floor muscles contract when you cough, sneeze or strain, helping to prevent the involuntary leakage of urine.
- They help to support the organs in your abdomen, especially when you are standing.
- They help to protect the pelvic organs from external damage.
- They help to hold the pelvic organs, like the bladder, in the correct position.
- They help in the control of passing of urine, gas, and bowel motions.
- They play a role in sexual function during intercourse.
In order for the pelvic floor muscles to carry out their function well, they need to be fit and adequately toned just like any other muscle in the body.
A weakness of the pelvic floor muscles may cause or worsen a number of problems including:
- Stress urinary incontinence. The complaint of involuntary loss of urine on effort or physical exertion, including sporting activities etc., or on sneezing or coughing.
- Urge urinary incontinence. The complaint of involuntary loss of urine associated with a sudden urgent need to pass urine.
- Mixed urgency and stress incontinence. The complaint of involuntary loss of urine associated with urgency and with effort or physical exertion, or on sneezing or coughing.
- Pelvic Organ Prolapse. Leading to a bulging of the bladder or bowel, or uterus (womb) into the vagina or out of the vaginal entrance if more severe.
- A loss in sexual sensation or feeling of vaginal looseness.
- Under use. Like all muscles, the pelvic floor muscles need exercise to work well. Regular and adequate intensive exercise of the pelvic floor muscles should be maintained all through life (not just after having children) and is therefore very important.
- Damage to the muscles during pregnancy and childbirth.
- The change in hormones associated with menopause might play a role in weakening the muscles but is still debatable.
- Decreased muscle tone with aging.
- Damage to the muscles through long term straining when constipated or associated with a chronic cough or obesity.
Intensive and regular pelvic floor exercises help by both strengthening and relaxing the pelvic floor muscles, so they become firm and supportive, but not overactive. Many women will have a major improvement in or recovery from symptoms of stress urinary incontinence by learning effective pelvic floor exercises, thus avoiding or delaying the need for surgery.
It is important to learn to do the exercises in the right way, and to check from time to time that you are still doing them correctly. Your therapist can help you to understand this by using diagrams, drawings and models.
- In the upright position, sit comfortably with your feet and knees wide apart. If preferred, you can also lie down flat (supine position) with your legs slightly apart. Remember to keep breathing throughout and keep your stomach, leg and buttock muscles relaxed.
- Imagine that you are trying to stop yourself from passing gas from the bowel and at the same time trying to stop the flow of urine from the bladder. You should feel a lifting and tightening around the vagina and anus.
- Observing the muscles can be an effective way of checking they are working correctly. Lie propped on the bed; place a small mirror between your legs with your knees bent and apart. As you pull up the pelvic floor you should see your anus and entrance to the vagina lifting and drawing in.
Note: If you notice the entrance to the vagina widening, you are pushing down and not pulling up, which is the opposite to tightening the pelvic floor muscle. Also, if you leak urine or pass gas when doing the exercises it is likely you are pushing down not pulling up.
You may not be able to immediately contract and relax adequately at first. Don’t be disappointed. Most patients will learn to contract and relax if they are given some time by themselves at home to practice.
How often should I practice?
First determine your ‘starting block’. Use your diary.
Tighten your pelvic floor muscles maximally without using your buttocks or thigh muscles as described above. Hold tight for as many seconds as you can (up to a maximum of 10 seconds).
How long can you hold the maximal contraction?
_______ secs
Release the contraction and rest for at least the same time of the contraction. Repeat the ‘tighten, hold and release’ as many times as you can (up to a maximum of 8-12 repetitions)
How many times can you repeat the contraction?
_______ times
e.g. 2 secs, 4 times
This becomes your ‘starting block.’ Repeat your starting block 4-6 times during the day. As a result of this muscle training, your pelvic floor will get stronger and your starting block will change.
e.g. 4 secs 6 times
This becomes your new starting block.
This program builds up the endurance of the muscle group. In other words, the muscle will be able to work harder for longer.
Now perform the pelvic floor exercise, but squeeze quickly and then let go. Rest 1-2 seconds before the next one. These are called quick contractions and will help your muscles react quickly when you laugh, cough, exercise or lift.
How many contractions can you do?
Aim to increase this number to 8-12 contractions, 3 times a day for at least 6 months. That’s the easy bit! The most difficult part of the program is remembering to do the exercises! Here are some tips to help trigger your memory:
- Wear your watch on the wrong wrist.
- Put stickers in places that will catch your eye (e.g. bathroom mirror, telephone, fridge, kettle, steering wheel).
- Exercise after you have emptied your bladder.
- Exercise in any position.
You may not feel your bladder control improve until after 3-6 weeks, but it may take up to 6 months to have improvement. DON’T GIVE UP!!
It is important to maintain the strength of the muscles once you have completed an exercise programme. Practicing your exercises twice a week, 3 sets of 8-12 maximal contractions, 3 times a day should be sufficient. Try to incorporate these exercises into daily life activities. If you are not sure that you are doing the exercises correctly ask your family doctor, nurse, physiotherapist or continence nurse to check for you.
If you are unable to contract your muscles, your health professional may suggest some additional treatments.
Biofeedback- This aims to help women identify and contract and relax selectively the pelvic floor muscles using signals from their own bodies. Feeling the muscles with your fingers is one example of this. Other methods involve using small sticky electrodes placed on the abdomen and buttock area or an intra-vaginal or intrarectal probe connected to a computer. The strength and length of the contraction you perform can then be seen on the computer screen.
Electrical Stimulation Therapy- Sometimes the pelvic floor muscles cannot (yet) contract due to nerve damage, e.g. from the delivery of a baby or after surgery. Electrical stimulation will provide an artificial contraction of the pelvic floor muscles, so helping to strengthen them. This method is not suitable for women who can already contract their pelvic floor muscles even if those contractions are weak.
- Weak pelvic muscles often cause bladder control problems.
- Daily intensive exercises can strengthen pelvic muscles and improve bladder control.
- Ask your therapist whether you are squeezing the right muscles.
- Always tighten and contract your pelvic muscles before coughing, sneezing, jumping or lifting. This can help prevent involuntary loss of urine, gas or stool, or bulging down of your pelvic organs.
- Try to maintain your weight within healthy limits.
Please visit this page to view instructional videos.
