Anterior Vaginal Repair
Introduction
About 1 in 10 women will require surgery for vaginal prolapse. A prolapse of the front (anterior) wall of the vagina is usually due to a weakness in the strong tissue layer (fascia) that divides the vagina from the bladder. This weakness may cause a feeling of fullness or dragging in the vagina or an uncomfortable bulge that extends beyond the vaginal opening. It may also cause difficulty passing urine with a slow or intermittent urine stream or symptoms of urinary urgency or frequency. Another name for an anterior vaginal wall prolapse is a cystocele.
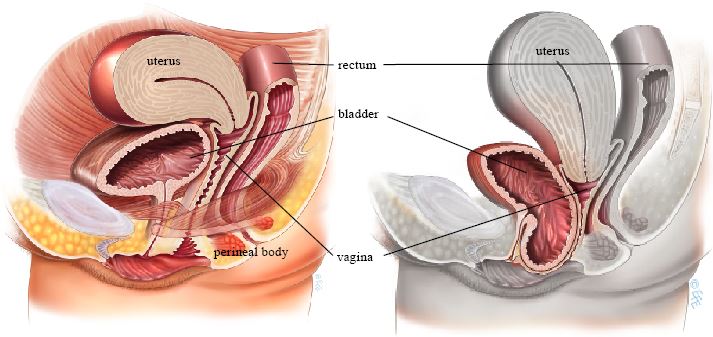
Normal anatomy, no prolapse (left) and Anterior wall prolapse (right)
In this Health Topic
An anterior vaginal wall repair, also known as an anterior colporrhaphy, is a surgical procedure to repair or reinforce the fascial support layer between the bladder and the vagina.
The aim of surgery is to relieve the symptoms of vaginal bulge and/or laxity and to possibly or potentially improve bladder function without compromising sexual function.
The surgery can be performed under general, spinal or even local anesthetic. Your doctor will discuss which is best for you. There are many ways to perform an anterior repair. Below is a general description of a common repair method.
- An incision is made along the center of the front wall of the vagina starting near the vaginal entrance and finishing near the top of the vagina.
- The vaginal skin is then separated from the underlying supportive fascial layer. The weakened fascia is then repaired using absorbable stitches, which will absorb over 4 weeks to 5 months depending on the type of stitch (suture) material used.
- Sometimes excessive vaginal skin is removed. The vaginal skin is closed with absorbable sutures. These usually take 4 to 6 weeks to fully absorb.
- A cystoscopy may be performed to confirm that the appearance inside the bladder is normal and that no injury to the bladder or ureters has occurred during surgery.
- A pack (long piece of gauze) may be placed into the vagina and a catheter into the bladder at the end of surgery. If so, this is usually removed within 24 hours of the surgery. The pack acts like a compression bandage to reduce vaginal bleeding and bruising after surgery.
- An anterior vaginal wall repair surgery can be combined with other surgery such as a vaginal hysterectomy, a posterior vaginal wall repair or incontinence surgery if indicated. These procedures are covered in detail in other leaflets in this series.
You will be asked about your general health and medication that you are taking. Any necessary investigations (for example, blood tests, ECG, chest x-ray) will be organized. You will also receive information about your admission, hospital stay, operation, pre- and post-operative care.
After the operation you may have a drip to give you fluids and may have a catheter in your bladder. The surgeon may have placed a pack inside the vagina to reduce any bleeding into the tissues. Both the pack and the catheter are usually removed within 24 hours of the operation. It is normal to get a creamy discharge for 4 to 6 weeks after surgery. This is due to the presence of stitches in the vagina. The discharge will gradually reduce as the stitches are absorbed. If the discharge has an offensive odor contact your doctor. You may get some blood-stained discharge immediately after surgery or starting about a week after surgery. This blood is usually quite thin and old, brownish looking and is the result of the body breaking down blood trapped under the skin.
Quoted success rates for anterior vaginal wall repair are 70-90%. There is a chance that the prolapse may come back in the future, or another part of the vagina may prolapse for which you need further surgery.
With any surgery there is always a small risk of complications. The following general complications can happen after any surgery:
- Anesthetic problems. With modern anesthetics and monitoring equipment, complications due to anesthesia are very rare.
- Bleeding. Serious bleeding requiring blood transfusion is unusual following vaginal surgery (less than 1%).
- Post-operative infection. Although antibiotics are often given just before surgery and all attempts are made to keep surgery sterile, there is a small chance of developing an infection in the vagina or pelvis.
- Bladder infections (cystitis) occur in about 6% of women after surgery and are more common if a catheter has been used. Symptoms include burning or stinging when passing urine, urinary frequency, and sometimes blood in the urine. Cystitis is usually easily treated by a course of antibiotics.
The following side effects are more specifically related to anterior vaginal wall repair.
- Damage to the bladder or ureters during surgery is an uncommon complication which can be repaired during surgery.
- After a large anterior vaginal wall repair some women may develop stress urinary incontinence due to the unkinking of the urethra (tube from the bladder). This can usually be resolved by doing pelvic floor exercises (as taught by a specialist pelvic floor physiotherapist) or by surgery to support the urethra (see the leaflet on stress urinary incontinence).
- Some women develop pain or discomfort with intercourse (dyspareunia). While every effort is made to prevent this from happening, it is sometimes unavoidable. Some women also find intercourse is more comfortable after their prolapse is repaired.
- Constipation is a common post-operative problem, and your doctor may prescribe laxatives for this. Try to maintain a high fiber diet and drink plenty of fluids to help as well.
In the early post-operative period, you should avoid situations where excessive pressure is placed on the repair, i.e., lifting, straining, vigorous exercise, coughing, and constipation. Maximal strength and healing around the repair occur at 3 months and care with heavy lifting (>10kg/25lbs) needs to be taken until this time. It is usually advisable to plan to take 2 to 6 weeks off work. Your doctor can guide you as this will depend on your job type and the exact surgery you have had. You should be able to drive and be fit enough for light activities such as short walks within 2 to 3 weeks of surgery. You should wait 5 to 6 weeks before attempting sexual intercourse. Some women find using additional lubricant during intercourse is helpful. Lubricants can easily be bought at supermarkets or pharmacies.
