Mesh: Mid-urethral Slings
FREQUENTLY ASKED QUESTIONS
- Mesh: Mid-urethral Slings
- What is mesh?
- Are there other areas in the body where mesh is used?
- Does polypropylene cause auto immune disorders?
- What is the difference between a mid-urethral sling and vaginal prolapse mesh?
- When is a mid-urethral sling used for treating SUI?
- How does a mid-urethral sling work?
- How successful are mid-urethral slings for treating SUI?
- What if I have urge incontinence as well?
- I have a mid-urethral sling inserted and I’m fine, but I’ve heard worrying reports in the news. Should I have it removed?
- What are the possible complications of mid-urethral sling surgery for SUI?
- What is mesh exposure?
- How common is mesh exposure?
- What symptoms might I experience if mesh becomes exposed?
- Are there any risk factors for mesh exposure?
- If I have mesh exposure can it be treated?
- I’ve heard women can get severe pain following mesh surgery for SUI. How is this addressed?
- Are there non-surgical options for treating SUI?
- Are there other surgical options to treat stress urinary incontinence?
Introduction
In response to the huge amount of media coverage regarding mesh used for the repair of pelvic organ prolapse and stress urinary incontinence, we have provided answers to frequently asked questions. We hope you find this information useful.
In the media there is often a confusion between mesh placed for the management of prolapse and the thin strip of mesh used to treat stress incontinence. Internationally, doctors make a clear distinction between surgical meshes placed vaginally for the treatment of pelvic organ prolapse and the mid-urethral slings (or tapes) used to treat women with stress urinary incontinence (SUI) as the risks and benefits of the procedures differ significantly.
SUI is leakage associated with coughing and exercise. It is common, affecting up to one in three women. Urinary incontinence can have a very significant impact on a woman’s quality of life, affecting her ability to exercise, cough, sneeze, enjoy intimacy, and can result in a loss of self-confidence. Buying pads to contain leakage is expensive.
Mesh sling procedures for stress urinary incontinence have been used for over 25 years and are the most widely used surgical treatment for stress incontinence worldwide. In international surveys, mid-urethral slings were the preferred method of treatment for stress urinary incontinence by more than 95% of surgeons.
What is mesh?
Surgical mesh is a synthetic material made from woven polypropylene. It is used as a support for damaged or weakened tissue.Are there other areas in the body where mesh is used?
Yes. Mesh has been used for many years in the treatment of hernias, and as a suture material for fifty years.
Does polypropylene cause auto immune disorders?
No. Despite media reports, there is no scientific evidence that the polypropylene is associated with any autoimmune disorders.
What is the difference between a mid-urethral sling and vaginal prolapse mesh?
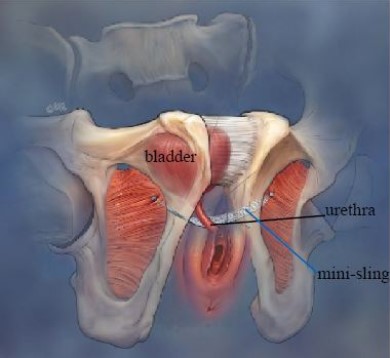
A mid-urethral sling (MUS) is used to treat stress urinary incontinence and is a narrow, 1-centimeter strip of mesh placed under the urethra (tube that drains the bladder). With the help of small needles, the sling is placed in one of three ways:
As a retropubic sling where the tape sits closely between the pubic bone and bladder:
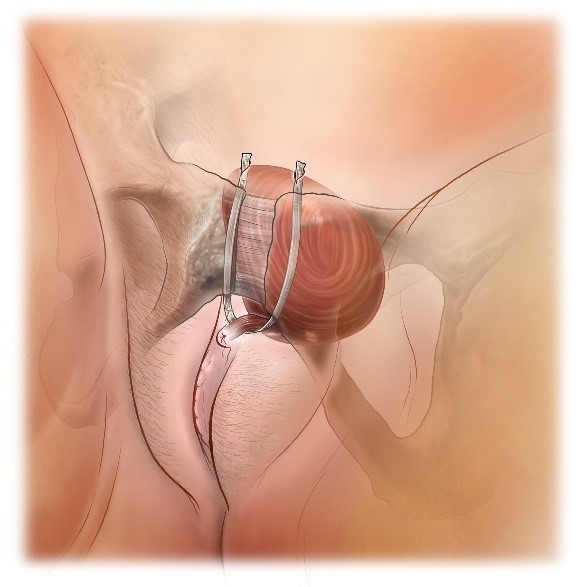
As a transobturator sling that passes out through small incisions in the groin:
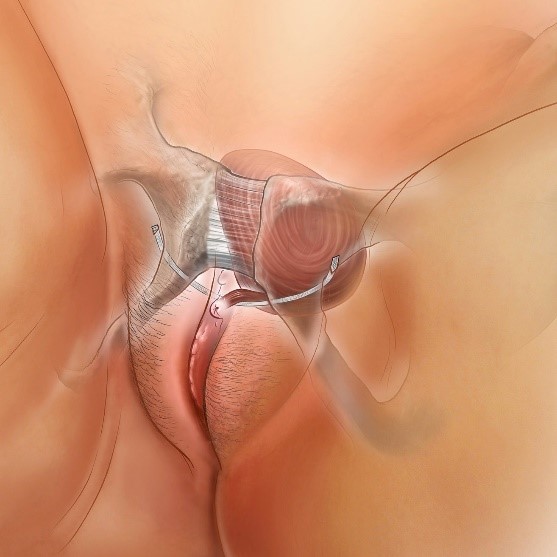
As a mini sling that is smaller and has no exit points:
For more information on each type of sling, please refer to our patient leaflet on mid-urethral slings available at www.YourPelvicFloor.org.
Mesh used for vaginal prolapse is a much larger piece than that used for SUI and is in the form of a small sheet rather than a tape. The mesh is placed under the vaginal skin to help cure vaginal bulge (prolapse). To keep the mesh in place, most have two or four “arms” which pass through the pelvis. In the past much larger and heavier-weight pieces of mesh were used compared to those currently available.
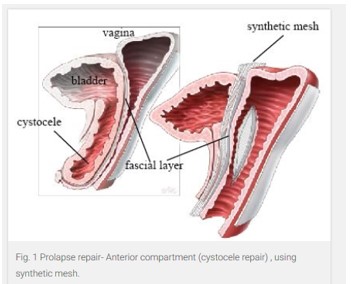
A large number of countries have now recommended that mesh inserted vaginally for pelvic organ prolapse should only be used in special cases, for example when a prolapse is very severe or traditional surgery has failed. Mesh is usually only placed to support the wall between the vagina and bladder, as mesh placed between the rectum and vagina has not been found to be better than traditional surgery. Some countries, like Australia and New Zealand, have gone further and restricted or discontinued the use of vaginal mesh for prolapse repair, while in the United Kingdom its use is currently suspended.
When is a mid-urethral sling used for treating SUI?
When simple measures like pelvic floor exercises and lifestyle changes have failed to cure urinary incontinence, surgery may be needed. A mid-urethral sling procedure would be considered as an option in this situation.
How does a mid-urethral sling work?
Mid-urethral slings are placed under the middle portion of the urethra through a small 1-centimeter cut in the vaginal skin. Within 3 to 4 weeks of sling placement, scar tissue develops around the sling and the body grows tissue through the sling. The combination of the sling and scar tissue strengthens and supports the area of weakness under the urethra to reduce or stop urine leakage.
How successful are mid-urethral slings for treating SUI?
Success rates following mid-urethral sling surgery for SUI are up to 85%. Even if complete dryness is not achieved, the severity of leakage is almost always much less. Large scientific studies from around the world have supported the safety and efficacy of the mid-urethral sling.
What if I have urge incontinence as well?
Urge incontinence refers to the urgent need to pass urine that results in leakage. Some women have triggers for this, such as hearing a running tap or placing the key into the front door. Mid-urethral slings are not designed to fix urge incontinence. Treatment for this involves lifestyle changes, bladder training, and medications or Botulinum Toxin.
Although mid-urethral slings are not designed to fix urge incontinence, about 45% of women will have an improvement in their urge symptoms, 4-5% may get a worsening of urge symptoms, and 50% will not experience any change following surgery with a mid-urethral sling.
I have a mid-urethral sling inserted and I’m fine, but I’ve heard worrying reports in the news. Should I have it removed?
No. If you are feeling fine and have no symptoms, there is no need to do anything; you do not need to remove the mesh sling. Additionally, removal of mesh that is not causing any problems can actually lead to a return of incontinence. Recent evidence has also confirmed that there is no increased risk of cancer or autoimmune disorders with mesh sling placement and mesh does not break down, disintegrate, or degenerate in the body.
What are the possible complications of mid-urethral sling surgery for SUI?
Possible complications include bleeding, injury to surrounding blood vessels or perforation (making a small hole in the bladder), urinary tract infections, difficulty passing urine, and pain. Pain is usually mild and lasts a few days but for some women pain may be severe and require the removal of the sling. Pain is more common following a transobturator sling procedure and can present as groin pain, pain with walking or squatting, or a burning nerve-type pain. Other women may experience vaginal pain or discomfort. In 2-4% of cases, the small incision through which the sling was placed may not heal well, leaving the sling exposed.
What is mesh exposure?
Mesh exposure is the term used to describe when a sling that has been placed is visible at the skin surface. Mesh exposure may occur early after a mesh is placed due to a failure of a surgical incision to heal well. In some cases, the mesh exposure may not occur until a later date. Other terms you may have heard used for mesh exposure include mesh erosion or extrusion.
How common is mesh exposure?
The mesh exposure rate for incontinence procedures using a mid-urethral sling is reported to be 2-4%.
The reported mesh exposure rate for vaginal mesh for prolapse surgeries is higher, at least 10% (1 in 10 women). This is a particular problem with older mesh types that are no longer used. Newer light-weight meshes used in prolapse surgery have an exposure rate less than half that of older products.
What symptoms might I experience if mesh becomes exposed?
You may have no symptoms at all or may notice a vaginal discharge which could be pinkish in color. Some women may feel the mesh as a roughness in the vagina or their partner may feel the mesh during intercourse.
Are there any risk factors for mesh exposure?
Research has shown that older women and women suffering with diabetes, obesity, or who smoke have an increased risk of mesh exposure. In addition, women who have had previous scarring and vaginal surgery, or who have longer surgical incisions during mesh placement, are also at increased risk.
If I have mesh exposure can it be treated?
Mesh exposure following a mid-urethral sling procedure is usually easy to manage either by re-covering the exposed sling with the surrounding tissue or by trimming the exposed piece. This sort of procedure can usually be done in the office under local anesthesia. If a mid-urethral sling needs to be trimmed it may reduce its effectiveness and the symptoms of stress incontinence could return.
I’ve heard women can get severe pain following mesh surgery for SUI. How is this addressed?
It is important to remember that pain as a complication can occur with any pelvic surgery, whether mesh is used or not. Mid-urethral slings can occasionally cause pain in the vagina, the legs/groin, and/or abdominally. Usually when this occurs it is because the mesh was placed too tightly or is healing with a lot of scarring, resulting in a pulling on the muscles and nerves and causing irritation to these structures. In addition, as with any pelvic floor surgery, on rare occasions a direct nerve injury may occur which can cause pain as well. Women who suffer with pain conditions such as fibromyalgia are at an increased risk of developing pain after a sling insertion.
The most important thing is to recognize the problem and get treatment early. Pain is a complication that can be treated in most cases if properly managed. A conservative (non-surgical) approach can be used first, however, if the pain does not improve or is very severe (which may be a sign of nerve injury), a surgical approach may be indicated.
What is conservative therapy?
Conservative therapy may involve using pain killers or pelvic floor physical therapy (i.e. manual therapy on the muscles and the nerves in the vagina and pelvis to help them relax or relieve spasm that may be causing pain). Sometimes trigger point injections, e.g. Botulinum Toxin, are recommended to relieve muscle spasm. If pain is due to the position of the tape or pain does not settle with conservative therapy, your doctor may recommend surgical removal.
Surgical Therapy
If conservative therapy has failed, your doctor may recommend surgery. Your doctor will carefully perform a pelvic examination to look for areas of tenderness and scar banding and for pressure points that may mimic the pain. Identified trigger points can be treated by releasing the tension through a small vaginal incision and/or removing part or all of the sling. If pain is experienced in the groin or on walking, or a nerve has been irritated in the groin, pelvis or abdomen, your doctor may recommend completely removing the sling. Removal of retropubic and mini slings is relatively straightforward while removal of a transobturator sling is more complex. Make sure your doctor has experience in managing and removing mid-urethral slings. Unfortunately, if there is a nerve injury, pain may become a chronic problem, even with total sling removal.
Are there non-surgical options for treating SUI?
Non-surgical treatments for stress urinary incontinence include pelvic floor muscle exercises and biofeedback. A pelvic floor therapist, or physiotherapist, can guide patients on how best to exercise and strengthen their pelvic floor muscles to help reduce their leakage.A recent scientific study found the mid-urethral sling to have a higher cure rate for stress urinary incontinence than pelvic floor physical therapy.
Another alternative to surgery is using support devices that are placed in the vagina to support the urethra. These are particularly helpful in cases in which leakage mostly occurs with specific activities, such as exercise. In those cases, the woman can insert the support device during those activities and remove it afterwards. Discussing your symptoms and desired treatment options with your doctor is helpful to tailor your treatment.
Are there other surgical options to treat stress urinary incontinence?
Various surgical procedures have been performed by surgeons for over 100 years to treat SUI. Such procedures include operating through abdominal or vaginal incisions with varying degrees of success. One such procedure is Burch colposuspension. Following an abdominal incision or using keyhole surgery, permanent stitches are placed on either side of the urethra and attached to supportive ligaments in the pelvis.
Autologous fascial slings are slings made from your own tissues. Surgery involves removing a strip of strong connective tissue (fascia) obtained from either the abdomen or thigh and using this to make a sling to support the urethra in a similar way to a mid-urethral mesh sling.
Depending on your circumstances, Burch colposuspension or autologous fascial sling procedures may be considered by your doctor as treatment options for stress urinary incontinence. However, the mid-urethral sling has been found to be as effective or more so than either of these procedures and is as durable, less complicated, and requires a shorter recovery time before returning to work.
In addition to surgeries designed to support the urethra, other surgeries have been developed to compress the urethra using bulking agents. Designed to be minimally invasive, they can be done in the office or with minimal anesthetic by injecting a bulking substance into the urethral lining to treat stress urinary incontinence. While neither as effective nor as durable as the mid-urethral sling for treating stress urinary incontinence, it is a good alternative in certain circumstances as it is well tolerated.
For detailed information on the Burch colposuspension, autologous fascial slings, and urethral bulking agents, please read our leaflets on these subjects here.
We do hope you have found the answers to these questions helpful. Remember your doctor would be happy to answer any other questions you might have. Writing down a list of your questions before visiting your doctor can be helpful. Finally, remember stress incontinence is not something you need to suffer with, and millions of women worldwide have been safely and effectively treated with mid-urethral slings.
