Fecal Incontinence (Accidental Bowel Leakage)
In this Health Topic
Fecal incontinence is the loss of control over bowel movements, resulting in the leakage of gas or stool (feces) through the anus (back passage). The severity of the symptoms can range from difficulty controlling gas to loss of control over liquid or formed stool. It is a common problem which can affect 7-15% of women at some time in their lives. It may result in bowel accidents caused by not being able to get to a toilet quickly enough (urge leakage) and soiling or leaking from the bowel without being aware of it (passive leakage).
Fecal incontinence can be distressing and can severely affect everyday life. Many people with fecal incontinence find it difficult and embarrassing to talk about it with healthcare professionals, their friends, or their families. However, once fecal incontinence has been identified, there are treatments available that can help manage or sometimes cure it, as well as strategies to help people cope with the condition and discuss it openly.
Normal bowel frequency varies between three times a day to two times a week, but most people have a bowel movement once a day. The Ideal consistency of stools is soft and formed. Normally, the bowel and rings of muscle around the back passage (anal sphincter) work together to ensure that bowel contents are not passed until you are ready. The sphincter has two main muscles which keep the anus closed: the inner ring (internal anal sphincter), which keeps the anus closed at rest, and the outer ring (external anal sphincter), which provides extra protection when the urge to open the bowel is felt and when we exert ourselves, cough or sneeze (Figure 1). These muscles, the nerves supplying them, and the sensation felt within the bowel and sphincter all contribute to the sphincter remaining tightly closed. This balance enables us to stay in control, or ‘continent.
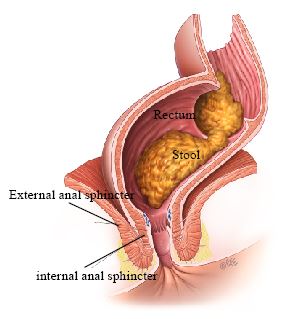
Internal & External Anal Sphincters
When stool enters the rectum, the internal anal sphincter muscle automatically relaxes and opens up the top of the anal canal. This allows the sensitive nerves at the top of the anal canal to detect whether it is gas, watery stool, or normal stool. The external anal sphincter can be deliberately squeezed to delay bowel emptying if it is not convenient to get to a toilet. Squeezing the
external sphincter pushes the stool out of the anal canal and back into the rectum, where the stool is stored until a convenient time (Figure 2).
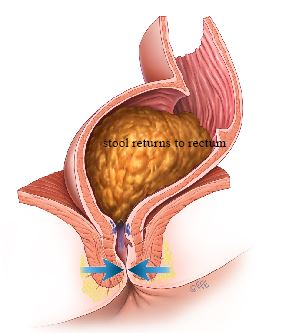
External anal sphincter contracting
Fecal incontinence occurs most commonly because the anal sphincter is not functioning properly. Damage to the sphincter muscles or to the nerves controlling these muscles, decreased muscle strength, excessively strong bowel contractions, or alterations to bowel sensation can all lead to disturbance of normal anal sphincter function.
One of the most common causes of fecal incontinence in women is injury during childbirth. The anal muscles may be torn during delivery or there may be damage to the nerves that help the anal muscles function. Some of these injuries can be recognized at the time of delivery, but others may not be as obvious and only become a problem later in life.
Some individuals experience loss of strength of the anal muscles as they age, so fecal incontinence may become more of a problem with advanced age. Anal surgery or injury to the area around the anal muscle can also lead to a loss of bowel control.
Certain groups of people are more likely to have fecal incontinence than others. Healthcare professionals should ask people in the groups below (or their caregivers) if they experience fecal incontinence:
- New mothers – usually due to a tear (hidden or obvious) in the sphincter muscles
- People of any age who experience an injury or infection of the sphincter; they may be affected immediately or later in life
- People suffering from Inflammatory Bowel Disease (colitis) or Irritable Bowel Syndrome (alternating diarrhea and constipation together with abdominal pain) because the bowel is overactive and squeezes strongly
- People who have had an operation on their colon (part of the bowel) or anus
- People who have had radiotherapy to their pelvic area
- People who have had a prolapse (slippage of the organ from its normal position in the body) of their rectum or pelvic organs
- People who have injury to, or disease of, their nervous system or spinal cord, such as multiple sclerosis
- People with learning disabilities or memory problems
- Children and teenagers who were born with an abnormal sphincter or who have persistent constipation
- Frail or elderly people
- People with urinary incontinence
An initial discussion with your doctor is the first step in assessing fecal incontinence. This discussion will help establish the degree of difficulty you have controlling your bowel movements and how it is affecting your lifestyle. By reviewing your history, your doctor may be able to identify the cause of the incontinence. For example, childbirth history – such as multiple births, large birth weight, forceps or vacuum-assisted deliveries, episiotomy or vaginal tears – is very important in determining possible causes. In some cases, bowel conditions, medical illnesses, and medications can play a role in loss of bowel control. If you are taking any medicines, your healthcare professional should consider whether this is making your incontinence worse, and if so, offer a different treatment if possible.
A physical examination of the anal area should be performed. An obvious defect (gap) or injury can be readily assessed. Tests of sphincter function are relatively simple to perform and are usually pain-free. The strength of the muscles, sensation, and nerve function, for example, can all be tested using simple pressure measuring devices. An ultrasound using a thin probe in the anal canal or placed against the perineum (area between the vagina and the anus) can provide a picture of the anal sphincter muscle rings and look for any disruption, thinning, damage, or defect (gap) in the anal muscles. Further tests may be needed depending on your situation.
As part of your assessment, you should be given advice to help you deal with your incontinence. Your healthcare professional should tell you about continence products available and how to use them, including disposable pads. Advice on cleaning and protecting your skin to prevent it from getting sore as well as advice on odor control and how to deal with your laundry should also be given.
It is possible to regain control of your bowel. While this may seem difficult at times, there are many simple and effective treatments available. You may need to work with a specialist who has expert knowledge about fecal incontinence. The following measures will help you manage your symptoms and regain control.
Simple self-help measures
Diet / bowel habits
The type of food you eat and the amount of fluid you drink impact the frequency of bowel movements and the firmness of your stools. You may be asked to keep a diary of your food and fluid intake. You should eat a healthy balanced diet and drink between 1.5-2 liters of fluid per day (6-8 cups). Water is the best fluid. Caffeinated drinks should be kept to a minimum. It is worth experimenting with your diet to see if certain foods or liquids, such as caffeine or alcohol, worsen the situation. Ensuring you have bowel movements at regular times during the day can help manage your fecal incontinence. If possible, use the toilet after a meal and make sure you have access to a private, comfortable and safe toilet facility that you can use for as long as you need. You should be advised about correct positioning, such as having your feet elevated off the ground with a small step or stool, when emptying your bowel (Figure 3). Straining or using abdominal pressure to push down should not be used when having a bowel movement.

Access to the toilet
Make sure you can use the toilet as easily as possible. A healthcare professional may assess your home and your mobility to see what extra help or equipment you might need to help you get to the toilet. If you are in a hospital or a care home, toilets should be easy to find and help to use the toilet should be available if you need it. Your privacy and dignity should always be respected.
Skin Care
Anyone who has frequent bowel movements, diarrhea, or accidental fecal leakage may get sore skin around the back passage. This can be very uncomfortable and distressing. Occasionally, the skin may become so inflamed that it breaks into open sores. These sores can be difficult to heal. Taking good care of the skin around your back passage can help to prevent these problems from developing. Tips to prevent soreness:
- After a bowel movement, wipe gently with soft toilet paper.
- Whenever possible, wash around the anus after a bowel movement. Use warm water only; disinfectants and antiseptics can sting if you have sores.
- After washing, gently pat your bottom dry with a soft towel (or soft toilet paper); do not rub.
- Avoid using products with a perfume on your bottom, such as scented soap, talcum powder, or deodorant Use a non-scented soap. Many baby wipes contain alcohol and should be avoided.
- Wear cotton underwear to allow the skin to breathe.
- Avoid tight jeans and other clothes which might rub the area
- Use non-biological washing powder for underwear and towels.
- Avoid using any creams or lotions on the area unless advised to do so.
- If you need to wear a pad because of incontinence, use a pad with a soft surface.
Pelvic floor / anal sphincter exercises
The pelvic floor is a sheet of muscles that extend from your tail bone to your pubic bone at the front, forming a “platform” between your legs. These muscles support the bladder, bowel, and uterus. The pelvic floor muscles help to control when you pass urine and open your bowel. Pelvic floor muscle exercises to improve the coordination and strength of the pelvic muscles can improve or stop any leakage from your bowel. If you opt for pelvic floor muscle exercises, a trained healthcare professional should plan a program with you, including regular assessment of your symptoms to see how well the exercises are working. Special exercises to strengthen the anal sphincter muscles help many people. Techniques such as biofeedback are now available to retrain the bowel to be more sensitive to the presence of stool so that the sphincter contracts when necessary. Such techniques are used in conjunction with physical therapy to improve bowel and pelvic floor coordination. In addition, electrical stimulation involving the application of tiny, safe electric currents to the anus in order to improve coordination and strength may also be added to the treatment.
Medication
Drugs may be helpful when:
- The bowel is squeezing too strongly resulting in urgency to get to the toilet quickly.
- The stool is very loose.
- The sphincter muscles are weak. Drugs can decrease movement in the bowel, making the stool more formed and the sphincter muscle tighter.
- Occasionally fecal incontinence is due to not emptying the bowel completely, and then use of suppositories or laxatives might be helpful.
Nerve Stimulation
Nerve stimulation is an outpatient treatment in which thin acupuncture-like needles are inserted into the skin above the ankle to stimulate the nerves involved in bowel and bladder function. It can be used to improve symptoms associated with accidental bowel leakage and fecal urgency. Around 1/3 of patients will experience a moderate improvement in episodes of bowel leakage, with more patients reporting an improvement in fecal urgency (an intense and sudden urge to have a bowel movement) and quality of life.
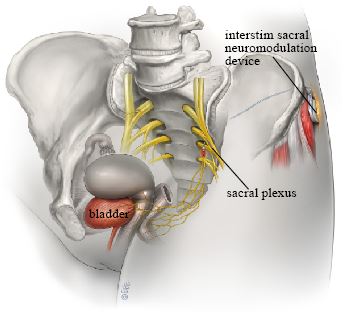
Sacral neuromodulation is another nerve stimulation treatment that uses electrical pulses to keep the anal sphincter closed. It is only suitable for people who have a weak but intact sphincter. It involves inserting electrodes under the skin in the lower back and connecting them to a pulse generator (Figure 4). This system produces pulses of electricity that are thought to affect the nerves controlling the lower part of the bowel and the anal sphincter, with the result that a person does not pass feces until he or she is ready to do so. There have been reports of good success with this method; 50 – 83% of people using the system see improvement or have no leakage. There is also evidence that quality of life improves once the sacral nerve stimulation system is in place.
Surgery
If your doctor thinks surgery might help you, he or she should refer you to a specialist surgeon. The surgeon should discuss the possible options with you, explaining the risks and benefits and how likely the operation is to work. The type of operation offered will depend on what is causing your incontinence. If you decide to have one of the operations, you should be offered ongoing support to help you. Available operations include:
- Anal sphincteroplasty involves repairing an injury or gap in the anal sphincter muscles
- Endoscopic radiofrequency (heat) therapy involves using heat energy to cause a degree of fibrosis (similar to scar tissue) to tighten the ring of muscle that forms the anal sphincter and help control bowel movements. It is intended to be less invasive than other surgical treatments and is usually done under sedation and local anesthetic.
- Antegrade irrigation involves washing out the colon withwater using a tube going through the wall of the abdomen into the appendix.
- Artificial anal sphincter implantation involves placing a circular cuff under the skin around the anus to allow you to control when you open your bowel.
- Stimulated graciloplasty involves making a new anal sphincter from muscle taken from the thigh. Electrical stimulation is applied to this new sphincter to strengthen it.
- Stoma. If there are no suitable treatments, your surgeon may consider offering you a stoma if you have incontinence that severely affects your everyday life. A stoma is an opening from your bowel through your abdomen, created by a surgeon. If this is the case, you will first be seen by a specialist stoma care service to explain all the risks, benefits, and long-term effects to you.
After each stage of your treatment, your healthcare professional should ask whether the treatment has helped you. If it hasn’t helped, you should be able to discuss and receive advice about other treatment options, including referral to a specialist. If you decide not to have any more treatment or your incontinence doesn’t improve, you should be offered options for practical and emotional support. In the very unusual situation that nothing can be done to decrease incontinence, appliances (such as an anal plug to insert in the anus to prevent fecal leakage) are available. Continence advisors and support groups may also offer emotional support and advice on navigating daily life with fecal incontinence.
