Nocturia
In this Health Topic
Nocturia is a condition which causes you to awaken many times (more than 2 times) during the night to urinate. This leads to sleep deprivation. Nocturia is more common as we age.
Nocturia is generally caused by polyuria (an excessive or abnormally large production of urine), low nighttime bladder capacity (not being able to hold enough in the bladder at night), or a combination of these.
Polyuria may be caused by:
- High fluid intake, especially in the evening.
- Untreated or poorly controlled diabetes. High blood sugar can make you thirsty and the resulting high fluid intake leads to polyuria.
- Congestive heart failure – a condition in which the heart does not pump blood through the body efficiently – can result in a large amount of fluid gathering in the legs and a decrease in blood flow to the kidneys, which is the cause of urine production during the day.
- Swelling of the legs as a result of fluid accumulation during the day. Once you lay down at night, the fluid shifts to the kidneys where urine is produced.
- Medications such as “water pills,” some heart medicines, demeclocycline, lithium, methoxyflurane, phenytoin, propoxyphene, and high dose Vitamin D.
Low nighttime bladder capacity may be caused by:
- Sleeping disorders which interrupt sleep, leading to more frequent bladder emptying during the night. This, over time, reduces the bladder’s ability to hold urine.
- Bladder obstruction (blockage) from spasm of the urethra, urethral stricture (partial blockage of the tube that empties the bladder), or a mass/tumor on the bladder or another pelvic organ.
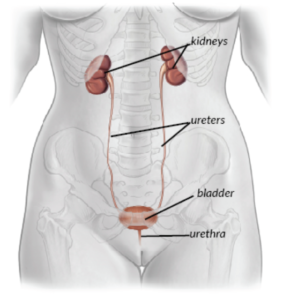
Figure 1: Urinary Tract
- Bladder spasm/overactivity (as in overactive bladder, with or without urge urinary incontinence – see www.yourpelvicfloor.org/conditions/overactive-bladder).
- Bladder infection, recurrent infection, or inflammation that causes the bladder wall to stiffen, often with shrinkage, irritation, and spasm. Eventually the bladder is unable to hold as much urine at night.
- Interstitial cystitis (Painful Bladder Syndrome – see www.yourpelvicfloor.org/conditions/interstitial-cystitis), which can cause bladder pain, in turn leading to the need to go to the toilet with greater frequency at night, just as it does during the day.
- Neurogenic bladder disorder, in which the nerve communicates abnormally to the bladder, causing abnormal filling and emptying.
Your healthcare provider will take a careful history, which will include your medical history and any medications you are taking. In addition to doing a physical examination, your provider will likely order a urinalysis (urine test) and ask you to complete a bladder diary.
Bladder Diary
A bladder diary (see www.yourpelvicfloor.org/conditions/bladder-diary-2) is a record of the fluids you drink, including when and how much, kept across a period of 2-3 days. You will also record when you urinate, how much you urinate, and if you experienced any urgency and/or urine leakage. This information helps your healthcare provider determine the possible cause(s) of your nocturia.
When you meet with your healthcare provider, you should be prepared to provide the following information:
- Approximate time the condition began
- Approximate number of times you urinate per night
- Amount you urinate at night (small, medium, large)
- Any recent changes in your urination habits
- Any diet changes (consumption of soda, spices, fluids, etc.)
- Any medications you are taking, including the dose and time of day you take each medication, or recent changes in medications you are taking
- Amount of alcohol and/or caffeinated beverages you consume and when
- Average number of hours of sleep you get per night (currently) and any recent changes in sleep habits
Treatment is dependent on the cause of the nocturia. If the cause is based on a disease, then the disease is treated. Otherwise, treatments fall into three categories: conservative approaches, medications, or surgical/procedural options. Conservative treatments are typically tried first.
Conservative Approaches:
- Restricting fluids, including caffeine and alcohol, especially after 4pm
- Taking “water pills” – preferably in the morning, but at least 6 hours before bedtime
- Elevating your legs above your chest, for example by using a recliner
- Wearing compression stockings
Medications:
- Desmopressin is the most commonly used medication for nocturia. It works by reducing the amount of urine produced at night. Most patients have no side effects, although headache or dizziness may occur. This medication requires regular blood tests to ensure you do not lose too much salt. Patients suffering from congestive heart failure cannot use this drug.
- Anticholinergic medications may be used to decrease bladder spasm, which tends to be present in most people experiencing nocturia. These medications will also decrease bladder spasm during the day. Side effects may include dry mouth or constipation. Sometimes anticholinergics are not recommended due to an increased possibility of confusion or falls in individuals over 65 years of age.
- Beta 3-adrenergic receptor agonists may relax the bladder muscle and increase bladder capacity with few side effects. It may be a first choice for elderly patients.
- Diuretic medications regulate urine production. These should be taken in the morning to cause maximum excretion of urine during the day and to decrease the amount urinated at night. Side effects are rare but may include headache and dizziness. Blood tests are recommended, as potassium supplements may be needed.
Surgical/Procedural Options:
- Bladder instillations (placing medications directly inside the bladder) can be done in the office. This is typically performed weekly for up to 6 weeks, based on symptoms.
- Injecting botulinum toxin A into the bladder wall through a tiny scope to relax the bladder muscle (outpatient procedure), if the cause of nocturia is non-responsive overactive bladder (see www.yourpelvicfloor.org/conditions/botulinum-toxin-a-bota-for-overactive-bladder-and-neurogenic-detrusor-overactivity).
- Placing a pacemaker-like device called a sacral neuromodulator to tell the bladder when and when not to contract, if the cause of nocturia is non-responsive overactive bladder.
- Bladder augmentation (adding on to the bladder) in very rare/special cases.
- Urinary diversion – a surgical procedure that reroutes urine through a new “bladder” usually made from your bowel.
This is a syndrome in which one has nocturia due to a hormonal disorder. Antidiuretic hormone (ADH) normally increases at night to prevent increased urination. Individuals with NPS have low levels or absent levels of ADH at night, which causes increased urination at night. The 24-hour urine output is normal. The treatment is replacement of ADH at night.
