Constipation
In this Health Topic
Constipation is a symptom, not a disease. Constipation means the bowel does not move easily or regularly. This may mean having a bowel movement fewer than three times a week and the stools (bowel motion) may be hard and difficult to pass.
Some people who are constipated find it painful to have a bowel movement and often experience straining, bloating, the sensation of a full bowel or a sense that the bowels are not empty. Some people think they are constipated if they do not have a bowel movement every day. However, normal bowel movements may vary from three times a day to about three times a week depending on the person.
Almost everyone experiences constipation at some point in their life. It is more common in women and adults ages 65 and older. Pregnant women may have constipation as the gut slows down in pregnancy, and it is a common problem following childbirth or surgery. Most constipation is temporary and not serious. Understanding its causes, prevention, and treatment will help most people find relief.
To understand constipation, it helps to know how the colon, or large intestine, works (Figure 1). The goodness and nutrients from food will have been absorbed higher in the gut, mostly in the small intestine, before the food moves into the colon. As food moves through the colon, the colon absorbs water from the food and forms it into stool. Mass waves of muscle contractions in the colon occur at intervals through the day and push the stool toward the rectum. By the time the stool reaches the rectum, most of the water has been absorbed and it should be formed and sausage-shaped, so it is easy to pass. Constipation occurs when the colon absorbs too much water or if the colon’s muscle contractions are slow or sluggish. This means the stool moves through the colon too slowly and as a result, stools can become hard and dry.
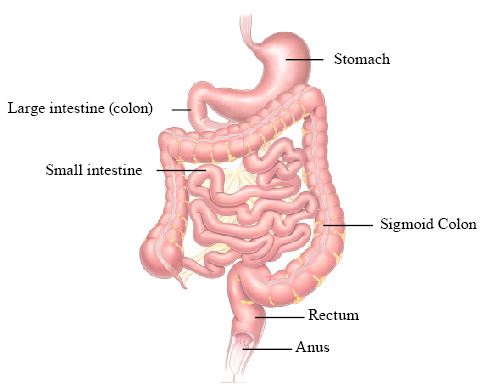
Digestive System
Common causes of constipation are:
- irregular meals and not enough fiber in the diet
- lack of physical activity (especially in the elderly)
- medications e.g., pain medications (especially narcotics), antacids that contain aluminum and calcium, some blood pressure medications (calcium channel blockers), anti-Parkinson drugs, antispasmodics, antidepressants, iron supplements, diuretics, anticonvulsants
- irritable bowel syndrome
- changes in life or routine such as pregnancy, aging, and traveling
- abuse of laxatives
- ignoring the urge to have a bowel movement
- dehydration
- specific diseases or conditions, especially those involving the nervous system such as stroke (most common)
- problems with the colon and rectum
- problems with intestinal function (chronic idiopathic or unknown reason for constipation)
Constipation can usually be diagnosed based on symptoms and a physical examination. Your doctor may also use the presence of any two of the following symptoms for at least 12 weeks (not always consecutive) in the previous 12 months as a guide:
- fewer than three bowel movements per week
- straining during bowel movements
- lumpy or hard stool
- sensation of incomplete emptying of your bowel
- sensation of anorectal blockage/obstruction
For most people a medical history and physical examination may be all that is needed for diagnosis and treatment. You should mention any medications you take regularly since some medications can cause constipation. You may need a rectal examination as part of a physical examination. A rectal examination involves inserting a gloved lubricated finger inside the rectum to feel for lumps or abnormalities. It can also check for blood in the stool.
Most people with constipation do not need extensive testing. The tests your doctor performs depend on the duration and severity of the constipation, your age, presence of blood in the stools, recent changes in bowel habits, weight loss or a family history of colon cancer. Testing may include blood tests, x-rays, sigmoidoscopy, colonoscopy, or more specialized tests (barium enema, defecography, colorectal transit study, anorectal function tests). Your doctor will explain a test to you if you need one, but you can also see the glossary of terms at the end of this leaflet.
Most people treat constipation at home, without seeing a healthcare provider. Self-treatment of constipation with over-the-counter laxatives is by far the most common aid. Around $725 million is spent on laxative products each year in America. It is important you speak with your doctor if the problem:
- is new (i.e., a change in your normal pattern).
- lasts longer than three weeks.
- is severe.
- is associated with any other concerning features such as blood on the toilet paper, weight loss, fever, or weakness.
Behavioral treatment
Lifestyle Changes
The bowels are most active following meals, particularly after breakfast. This is often the time when stools will pass most readily. Go to the toilet when you get the first sensation you need to open your bowels; don’t wait. If you ignore your body’s signals to have a bowel movement, the signals become weaker and weaker over time. Pay close attention to these signals and allow yourself enough time to have a bowel movement. A hot drink, e.g., tea or coffee, in the morning may stimulate the contractions of the gut and encourage a bowel movement, as does regular daily exercise.
Sitting properly on the toilet
The way you sit on the toilet can make a big difference to the ease with which your bowel empties. The correct position will improve the angle of the rectum (back passage), help your muscles to work efficiently, and prevent straining. You should aim for a ‘squatting’ type position on the toilet using the following technique:
- Sit comfortably on the toilet with your legs more than hip width apart.
- Place your feet flat on a footstool approximately 20cm high.
- Lean forward from the hips and rest your forearms on your thighs.
- Relax and breathe normally; you should not hold your breath.
- Make your waist wide by bulging your abdominal muscles outwards.
- Relax your anus.
- Use your abdominal muscles as a pump to push gently but firmly backwards and downwards towards your anus.
- Do not sit for longer than ten minutes. If your bowels have not opened, try again later.

Diet
Eating regularly and having adequate fluid intake are the most important factors for good bowel function. A diet with enough fiber (20 to 35 grams each day) helps the body form soft, bulky stool. However, for some people consuming large amounts of fiber can cause abdominal bloating or gas. Try to increase your fiber if needed by using more soluble fiber (fruits, vegetables, and oats) rather than insoluble (bran-type fiber). Start with a small amount and slowly increase until your stools become softer and more frequent. A doctor or dietitian can help plan an appropriate diet. By reading the product information panel on the side of the food package, you can determine the number of grams of fiber per serving (Table 1). Some foods have natural laxative properties such as prunes, figs, kiwi fruit, licorice, and molasses. Adding cracked linseeds and chia seeds to the diet may be beneficial to improving stool consistency and so making stool easier to pass. For people prone to constipation, limiting foods that have little or no fiber, such as ice cream, cheese, meat, and processed foods, is also important. To prevent dehydration and to help constipation, drink between 1.5 and 2.0 L of water or other liquids such as fruit/vegetable juices every day.
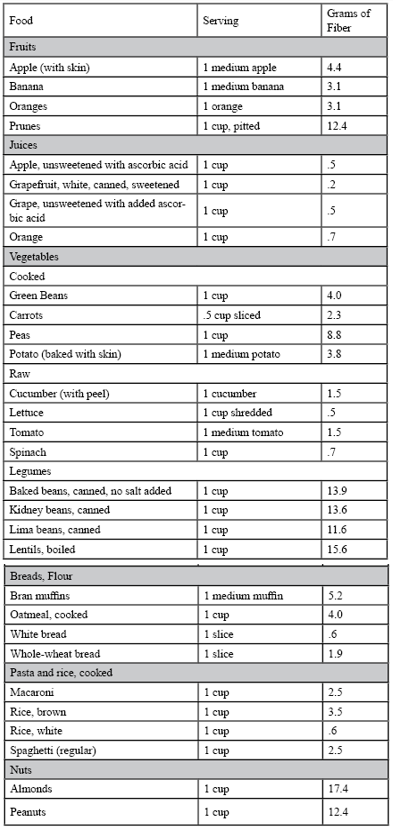
Table 1 – Amounts of Fiber in Different Foods
Medical Treatment
Treatment for constipation depends on the cause, severity, and duration of the problem. In most cases dietary and lifestyle changes will help relieve symptoms and prevent them from recurring. If these simple changes do not relieve your constipation, you may try the following treatments
Bulk-forming fibers
Bulk-forming fibers are generally considered the safest, but they can interfere with the absorption of some medicines. They include natural and commercial fiber preparations. They absorb water in the intestine and make the stool softer. The most well-known fiber supplement is called Psyllium Husk and you might be able to find it in your regular supermarket or pharmacy. Brand names include Metamucil, Fiberall, Citrucel, and Konsyl. They must be taken with plenty of water or they can cause obstruction. You should increase the dose of fiber supplements slowly to prevent bloating, gas and cramping.
Laxatives
In general, laxative use should be for occasional use only. Long term use of laxatives, particularly the stimulant laxatives, may lead to the bowel becoming less responsive. People who are dependent on laxatives need to stop using them gradually. For most people, stopping laxatives restores the colon’s natural ability to contract. A variety of laxatives are available for treating constipation. Choice is based upon how they work, how safe the treatment is, and your doctor’s preferences. In general, laxatives can be categorized into the following groups:
- Stimulant laxatives. These cause rhythmic muscle contractions in the intestines. Examples include senna (Senokot) and bisacodyl (e.g., Correctol, Dulcolax). However, it might cause abdominal cramps and diarrhea. Avoid overusing stimulant laxatives as taking them regularly or in large amounts can cause side effects.
- Osmotic laxatives. These cause fluids to flow in a special way through the colon and are especially useful for people with no underlying cause for their constipation (idiopathic constipation). Examples are polyethylene glycol (MiraLax), Lactulose and Sorbitol. Polyethylene glycol is generally preferred since, unlike lactulose and sorbitol, it does not cause gas or bloating. Sorbitol works as well as lactulose and is much less expensive. People with diabetes should be monitored carefully.
- Saline laxatives: These act like a sponge to draw water into the colon for easier passage of stool, similar to the osmotic laxatives. Examples include magnesium hydroxide (Milk of Magnesia) and magnesium citrate. Saline laxatives are used to treat acute constipation if there is no evidence of bowel obstruction.
- Suppositories and enemas: Apart from oral preparations (liquid, tablet, powder and granule), laxatives are also available as suppositories or enemas that you insert into the rectum. Many people do not like using them, but they do, in general, work more quickly than oral laxatives. When inserted into the rectum they soften the stool and cause the walls of the rectum to contract. Used at the same time of day they may also encourage a more regular bowel pattern. Occasionally prepackaged enema kits containing sodium phosphate/biphosphate (Fleet) may be recommended if you have not responded to other treatments. These are not recommended if you have problems with your heart or kidneys unless directed by your doctor.
Stool Softeners/Lubricants
Stool softeners moisten the stool to make it soft and easy to pass as it moves through the intestine more easily. They are often recommended after childbirth or surgery and for people who should avoid straining in order to pass a bowel movement. Stool softener brand names include Colace while mineral oil is the most common example of lubricant (brand names include Fleet). They typically stimulate a bowel movement within 8 hours, but prolonged use of these preparations should be avoided.
Other drugs
Chloride channel activators increase fluid and movement in the intestine to help stool pass, thereby reducing the symptoms of constipation. One such agent is Lubiprostone (Amitiza), a prescription medication that treats severe constipation and can be safely used for up to 6– 12 months. Thereafter, a doctor should assess the need for continued use. It is expensive compared to other agents, however, it may be recommended if you do not respond to other treatments.
Other treatments
Biofeedback
Biofeedback is a behavioral approach used by therapists and involves the use of a sensor to monitor muscle activity, which is displayed on a computer screen. This shows an accurate assessment of the muscle function and a therapist can help you to retrain the muscles controlling bowel movements. It may help some people with severe chronic constipation who involuntarily squeeze (rather than relax) their muscles while having a bowel movement.
Surgery
Surgery may be used to correct anorectal problems such as rectal prolapse, a condition in which the lining of the rectum bulges outward. Surgical removal of the colon may also be an option for people with severe symptoms caused by colonic inertia. However, the benefits of this surgery must be weighed against possible complications, which include abdominal pain, diarrhea and incontinence.
Sometimes constipation can lead to complications. These complications include hemorrhoids, caused by straining to have a bowel movement, and anal fissures (tears in the skin around the anus), caused by hard stool stretching the sphincter muscle. As a result, rectal bleeding may occur, appearing as bright red streaks on the surface of the stool. Sometimes straining causes a rectal prolapse to push out from the anal opening. This condition may lead to secretion of mucus from the anus. Usually eliminating the cause of the prolapse, such as straining or coughing, is the only treatment necessary. Severe or chronic prolapse requires surgery to strengthen and tighten the anal sphincter muscle or to repair the prolapsed lining. Constipation may cause hard stool to pack the intestine and rectum so tightly that the normal pushing action of the colon is no longer enough to expel the stool. This condition, called fecal impaction, occurs most often in children and older adults. An impaction can be softened with mineral oil taken by mouth and by an enema. After softening the impaction, the doctor may break up and remove part of the hardened stool by inserting one or two fingers into the anus.
Your doctor may use the following medical terms when discussing your condition:
Barium enema: This involves using x-rays to view the rectum, colon, and lower part of the small intestine to locate problems. The colon does not show up well on x-rays, so the doctor fills it with barium, a chalky liquid that makes the area visible. Once the mixture coats the inside of the colon and rectum, x-rays are taken that show their shape and condition. The patient may feel some abdominal cramping when the barium fills the colon but usually feels little discomfort after the procedure. Stools may be white in color for a few days after the test.
Defecography: An x-ray of the anorectal area to check how well stool is expelled. It will show the contraction and relaxation of the rectal muscles to check if they work correctly. During the test, the doctor fills the rectum with a soft paste that is the same consistency as stool. The patient sits on a toilet positioned inside an x-ray machine, then relaxes and tries to expel the paste as in a normal bowel movement.
Sigmoidoscopy or colonoscopy: A camera examination of the rectum and sigmoid (lower colon) is called a sigmoidoscopy while examination of the rectum and entire colon is called a colonoscopy. To perform a sigmoidoscopy, the doctor uses a long, flexible tube with a light on the end, called a sigmoidoscope, inserted through the anus. The patient is usually lightly sedated before the exam. The same procedure is used for colonoscopy, except the colonoscope tube is longer.
Colorectal transit study: This test shows how well food moves through the colon. The patient swallows capsules containing small markers that are visible on an x-ray. The movement of the markers through the colon is monitored by abdominal x-rays taken several times 3 to 7 days after the capsule is swallowed. The patient eats a high-fiber diet during the course of this test.
Anorectal function tests: These tests diagnose constipation caused by abnormal functioning of the anus or rectum.
- Anorectal manometry shows anal sphincter muscle function. A catheter or air-filled balloon is inserted into the anus and slowly pulled back through the sphincter muscle to measure muscle tone and contractions.
- Balloon expulsion tests consist of filling a balloon inserted in the anus with varying amounts of water. The patient is then asked to expel the balloon. The inability to expel a balloon filled with less than 150 mls of water may indicate a decrease in bowel function.
