Colposuspension for Stress Incontinence
Introduction
Stress incontinence is the complaint of involuntary leakage of urine following exertion or effort, e.g. coughing, sneezing or exercise. It is a very common and embarrassing problem affecting up to 1 in 3 women. Stress incontinence may be cured or improved with pelvic floor exercises and lifestyle modifications, but if these strategies fail then surgery may be available to you.
In this Health Topic
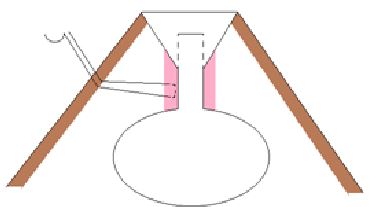
Colposuspension (also called Burch colposuspension) is an operation that involves placing sutures (stitches) in the vagina on either side of the urethra (pipe through which the bladder empties) and tying these sutures to supportive ligaments to elevate the vagina.
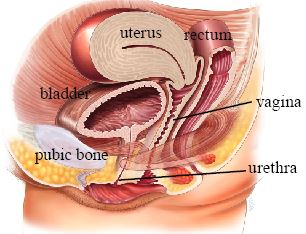
Normal Anatomy
Normally, the urethral sphincter and the muscles and ligaments around the urethra contract to prevent involuntary leakage of urine. Damage to these structures from childbirth and/or aging can lead to stress incontinence. The sutures in colposuspension elevate the vagina and support the urethra, thus reducing or stopping the leakage.
Most of the time, colposuspension is performed using an abdominal incision – a horizontal cut in the ‘bikini-line’. Some surgeons may perform the procedure laparoscopically or ‘keyhole’. During the operation, the bladder and urethra are identified and the space behind the pubic bone is exposed. Sutures are then placed in the tissue to the side of the urethra and attached to the iliopectineal ligament – a supportive tissue behind the pubic bone. A cystoscopy (a camera to view the bladder inserted via the urethra) is usually performed to ensure the sutures haven’t been placed in the bladder. A drain may be left behind the pubic bone to prevent a hematoma (a collection of blood) from forming. Additionally, a suprapubic catheter – inserted via the abdomen – may be introduced. The drain and catheter are left in for a couple of days. Your doctor will advise you when they will be removed.
Colposuspension
Colposuspension is usually performed under general anesthesia, although sometimes a spinal anesthetic may be offered. The anesthetist will discuss the best option for you prior to your operation.
One year following surgery, more than 80% of women will find that their stress incontinence has either improved or has been cured. Twenty years following surgery, approximately 60% remain satisfied with the outcome.
All operations are associated with risks of hemorrhage, infection, and venous thromboembolism (VTE). It is rare for transfusion to be required following colposuspension. The risk of acquiring infection is reduced by use of intravenous (IV) antibiotics when you are in the operating theatre. VTE generally involves a blood clot in the leg veins or in the lung veins and may present with leg pain/swelling, shortness of breath, cough, or chest pain. The risk of VTE is reduced by use of compression stockings and injections of blood thinners post-operatively to thin the blood. There are also risks associated with anesthetic which you can discuss with your anesthetist.
The specific risks of colposuspension include:
- Failure to work (up to 20% at 1 year).
- Overactive bladder symptoms (an urgent feeling to pass urine which may lead to incontinence) occur up to 17% of the time, however, some women may already have pre-existing bladder overactivity.
- Difficulty passing urine occurs in up to 10% of women. This usually improves but may be permanent. You may need to pass small catheters (clean intermittent self catheterization) to fully empty your bladder.
- Prolapse of the back vaginal wall (rectocele) affects 14% of women post-operatively.
- Difficulty with sexual intercourse may involve pain or a less intense orgasm due to the incisions and stitches in the vagina.
- Rarely, the stitches may erode into the bladder and require removal.
You should keep mobile to prevent the risk of VTE but avoid heavy lifting for the first few weeks after the surgery. Gradually build up your level of activity 6 weeks following surgery and by three months you will probably be back to normal. Do not use tampons or have sexual intercourse for 6 weeks following surgery. You may be apprehensive about resuming sexual relations and may need to take your time and use lubricants. Ensure you do not become constipated by drinking plenty of fluids and taking dietary fiber such as fresh fruits and vegetables, brown bread, and oats. Your doctor will advise you when you can safely drive again; this may be up to six weeks after the operation.
This operation is an option for women who are bothered by stress urinary incontinence. If the leaking does not bother you, you should not feel compelled to have surgery. Regular pelvic floor exercises are likely to reduce stress incontinence.
