Mid-urethral Sling (MUS) Procedures for Stress Incontinence
In this Health Topic
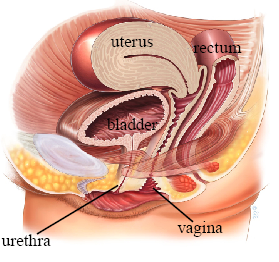
Mid-urethral sling (also known as tape) procedures are operations designed to help women with stress incontinence. Stress incontinence is the leakage of urine through the urethra (the tube through which urine is passed) with everyday activities such as coughing, sneezing, or exercise. It is a very common and embarrassing problem affecting up to 1 in 3 women. Normally the muscle and ligaments which support the urethra close firmly when straining or exercising to prevent leakage. Damage or weakening of these structures by childbirth and/or with age can result in this mechanism failing, leading to urine leakage. Stress incontinence may be cured or improved with pelvic floor exercises and lifestyle modifications, but if these strategies fail, then surgery may be recommended. The most frequently offered type of operation is a mid-urethral sling procedure, a simple outpatient procedure that has been performed on more than 3 million women worldwide.
The operation involves placing a sling made of polypropylene mesh (suture material that is woven together – about 1 cm wide) between the middle portion of the urethra and the skin of the vagina. Once the sling is in position, supporting connective tissue grows through the holes in the mesh weave to anchor the sling in position. This may take 3 to 4 weeks. The sling improves the support to reduce or stop urine from leaking.
Mesh sling procedures have been done safely for many years, however, in view of the recent media coverage of vaginal meshes, we have provided answers to frequently asked questions about meshes on our website (click here). Mesh sling procedures may not be available in all countries.
There are three main routes for placing the sling: behind the pubic symphysis (the retropubic route), next to the groin (the transobturator route), and using a “single incision” or “mini-sling.” The surgical route will depend on your doctor and the common practice in your part of the world.
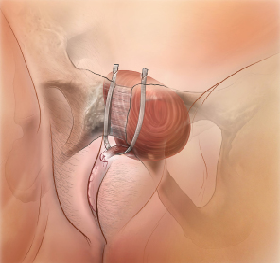
Retropubic Route (Tension-free Vaginal Tape or TVT)
In the retropubic approach, the sling is placed through a small cut made in the vagina. The two ends of the sling are passed on either side of the urethra to create a loose sling around the urethra. The ends exit through two small cuts just above the pubic bone on the lower abdomen which are often stitched closed with dissolvable sutures. The scars are usually discrete within the pubic hairline about 3-4 cm apart. The surgeon will then use a camera (cystoscope) to check that the sling is correctly positioned.
Research suggests that if this procedure is initially successful in controlling stress incontinence then it is still likely to be working up to at least 17 years later. For women with severe stress incontinence the retropubic route appears to be more successful than the other approaches.
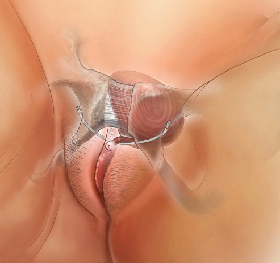
Transobturator Route (TOT)
For the transobturator approach, a small incision is made in the vagina and medial to the groin to pass the mesh sling so that the sling sits under the mid-portion of the urethra and the vagina. The sling passes through the obturator foramen, which is an opening between the bones of the pelvis.
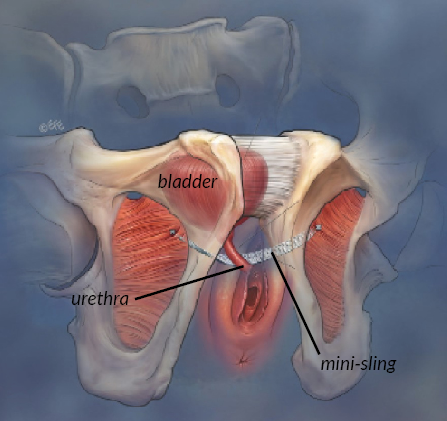
Mini-sling
Insertion of the mini-sling follows a similar pathway as the TVT mesh insertion or the TOT. The mini-sling uses a shorter strip of mesh to support the urethra and can have a small self-fixing anchor to keep it in place so no additional skin incisions are required. Mini-slings are less invasive than other methods, however long-term study results are lacking, and this may not be the best sling type for severe stress urinary incontinence.
This procedure can be carried out with you awake using local anesthesia or regional anesthetic (numb from the waist down), with a spinal anesthetic, or epidural. However, it is most commonly carried out with a strong sedative (deep sleep) or full general anesthesia.
Most surgeons will allow patients to go home after a mid-urethral sling operation once they are emptying their bladder well and after any pain has been adequately controlled. Normally this time will vary from a few hours to a couple of days. A catheter (tube inserted into the bladder to drain it) is not normally required following this procedure.
You should be fit enough for usual daily activities within a week of surgery. You are advised to avoid heavy lifting, sexual intercourse, tampon use, and sport for 6 weeks to allow the wounds to heal and the sling to be firmly held in place. Driving is not recommended until an emergency stop can be performed without pain, and you are free from any sedative effects of pain killers. Normally this is after 1-2 weeks.
Research tells us that, in the short term, this operation is as successful as other more invasive procedures used for controlling stress incontinence, but with a quicker recovery and less chance of needing repeat surgery. Between 80-90% of women are happy with their operation and feel that their incontinence is either cured or much better.
There is no completely “risk free” operation for stress incontinence. The likelihood of any of the following complications occurring is 1-10 per 100 patients.
Complications include:
- Urinary tract infections. These are common after any procedure and should respond to antibiotics. Symptoms of a urinary tract infection include burning, stinging, the need to pass urine frequently and in some cases bloody, cloudy, or offensive smelling urine. If you notice these symptoms contact your doctor.
- Bleeding. Bleeding sufficient to require a blood transfusion is very rare. Sometimes bleeding can happen where the tape from a retropubic operation passes behind the pelvic bones. This is normally self-limiting and only very rarely needs an operation to fix.
- Difficulty passing urine (voiding difficulty). Voiding difficulty may occur in 1-5% of patients, often because of swelling around the urethra or discomfort and will usually settle within a week. During this time your doctor may recommend a catheter (tube used to drain the bladder). If your urine stream remains very slow or you cannot empty the bladder well even after the swelling has settled, your care provider will discuss other possibilities, such as cutting or stretching the sling, with you.
- Mesh exposure. The mesh sling can appear in the wall of the vagina a few weeks, months, or years after an operation. Symptoms may include vaginal bleeding, vaginal discharge, or pain with intercourse for the patient or her partner. In such cases, you should consult your surgeon who will be able to advise you further. Management could involve prescription of oestrogen cream for the vagina, a small procedure to recover the tape, or removing the section of tape that is exposed or rarely removing the whole mesh tape. The risk of this happening is 2-4%.
- Bladder or urethral perforation. Bladder perforation more commonly occurs during TVT insertion (1-5%) compared with TOT placement. The urethra is at most risk of damage during a TOT procedure (1% or less). Cystoscopy at the time of sling insertion can identify this complication. If identified, the mesh sling will be removed and replaced in the appropriate position. The bladder is normally then drained by a catheter for 24 hours to allow the hole in the bladder to heal itself. If bladder perforation occurs and is recognized, it does not affect the success of the operation. Damage to the urethra is more difficult to deal with and should be discussed with your surgeon.
- Urgency and urge incontinence. Women who have bad stress incontinence often experience urgency and urge incontinence (leakage of urine associated with the sensation of urgency). About 50% of women notice an improvement in urgency symptoms, but for about 5% the symptoms may develop or worsen following a mid-urethral sling procedure.
- Pain. After the TVT insertion operation about 1% will develop vaginal or groin pain. Similar pain can occur in as many as 10% of women after a TOT procedure. In most cases pain is short lived and does not occur for more than 1 to 2 weeks. Rarely pain may not settle, and further treatment with full or partial removal of the sling may be required.
You should have the operation only if you feel the stress incontinence is affecting the quality of your life now, not to prevent it from deteriorating in the future.
Many surgeons would want to avoid surgery until a woman’s family is complete because future pregnancy may compromise the results of the initial surgery.
You are advised to wait for 4 weeks after the operation before having sexual intercourse. In the long term there is no evidence that the operation will adversely impact your sex life.
- Pelvic floor exercises (PFE). Pelvic floor exercises can be a very effective way of improving symptoms of stress urinary incontinence. Up to 75% of women show an improvement in leakage reduction after PFE training. The benefits of pelvic floor exercises are maximized if practice is carried out regularly. Maximum benefit usually occurs after 3 to 6 months of regular exercising. You may be referred to a physical therapist (physiotherapist) to supervise this. If you also have a problem with urge urinary incontinence your doctor may also advise bladder retraining exercises.
- Continence devices. Continence devices are available which fit in the vagina and help control leakage. These can be inserted prior to exercise or worn continuously. Some women find inserting a large tampon prior to exercise may prevent or reduce leakage. These types of devices are suitable for women with more mild to moderate stress urinary incontinence or who are waiting definitive surgical treatment.
- Lifestyle changes. If you are overweight, reducing weight can result in an improvement in incontinence symptoms. Maintaining good general health, quitting smoking, and having good control of medical conditions such as asthma can also be helpful.
- Alternative surgical procedures. Alternative surgical procedures include colposuspension, urethral bulking, autologous fascial sling insertion, or insertion of an artificial urinary sphincter. These options should be discussed with your doctor.