Fascial Slings
In this Health Topic
A fascial sling is a procedure performed to treat female stress urinary incontinence. Stress incontinence is the involuntary leakage of urine with everyday activities such as coughing, sneezing, or exercise. Stress urinary incontinence affects at least 20-30% of women. It can be very embarrassing and negatively affect quality of life. Many options for treatment are available, however, when other procedures have failed or the patient has concerns about using a synthetic material for their surgery (see leaflet on mid-urethral slings), then a fascial sling is a viable option.
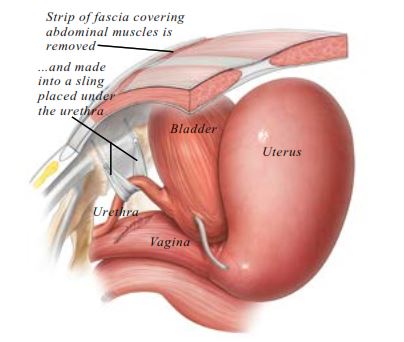
Fascial slings are made from the patient´s own fascia. The fascia is a layer of strong connective tissue usually obtained from the abdomen or thigh. The surgeon usually takes a strip of fascia 1-3cm wide and places it under the urethra (the pipe through which the bladder is emptied) to give support and reduce leakage of urine.
Most stress incontinence is caused by a lack of urethral support, usually due to raised intra-abdominal pressure (from pregnancy, childbirth, weight gain, etc.). A fascial sling is used to replace the damaged support structures.
The operation is done under anesthesia and involves two steps. First, the surgeon will take a strip of the fascia from the abdomen through a cesarean section-like incision, or from the thigh via a small incision.
Second, a small cut is made in the vagina, under the urethra. The strip of fascia is secured underneath the urethra and then passed up to the abdominal wall. Once the sling (fascia) is secured, the small cut in the vagina is stitched closed.
Towards the end of the surgery, most surgeons will routinely perform a cystoscopy. A cystoscopy allows the surgeon to look into the bladder using a telescopic camera to ensure no injury has been caused to the urethra or bladder (see leaflet on cystoscopy). A catheter is inserted to drain the bladder and this is usually removed the next day.
This procedure is usually done under anesthetic. Depending on your geographic location and health center, this can be general anesthesia, spinal, or epidural.
Most surgeons will allow patients to go home once they are sure the patient is emptying their bladder efficiently. This may vary from one to a couple of days.
You should be able to drive and be fit enough for usual daily activities within 4-6 weeks of surgery. After surgery it is advisable to avoid heavy lifting, sexual intercourse, and sport for 6 weeks to allow the wounds to heal.
Current data suggest fascial slings are as successful as synthetic mid-urethral slings. The overall success rate varies from 80 to 90% for a first operation. Most women feel their stress incontinence is either cured or much better following the procedure.
There is no completely risk-free operation for stress incontinence. There are a number of general risks related to surgery and anesthesia including wound infections, urinary tract infections, blood clots in the legs or lungs, and pain/discomfort following the operation. Complications specific to fascial sling surgery include:
- Bleeding. Sometimes bleeding can occur from the passing of the needle behind the pubic bone, causing a hematoma (collection of blood). Bleeding sufficient to require a blood transfusion is very rare. You can expect some light vaginal bleeding for up to a few weeks.
- Difficulty passing urine (voiding difficulty). Some women have difficulty emptying their bladder following sling surgery, which can take up to 6-8 weeks to resolve. Some patients may be discharged with an indwelling catheter. If, following a reasonable amount of time, you continue to have problems emptying your bladder, the surgical team will discuss options with you which may include learning to self-catheterize, loosening the sling or removing it all together. This occurs in about 5% of women.
- Fascial exposure. Exposure of fascial slings following surgery is rare in fascial slings where the patient’s own connective tissue is used (compared with mid-urethral slings). However, wound healing may be affected by infection, smoking, and use of steroids. If the fascial tissue is exposed and causing the patient or her partner symptoms or pain, then the sling will usually be removed.
- Bladder or urethral damage. Bladder damage may occur during the passage of the needles through the space behind the pubic bone. To address this, the needles are removed and relocated in the correct position. The bladder is normally then drained by a catheter for 24 hours to allow the hole in the bladder to heal. The bladder usually heals itself within a few days. Damage to the urethra is rare but more difficult to deal with; your surgeon will explain how this is managed should it occur.
- Urgency and urge incontinence. Women who have stress incontinence may also experience urgency and urge incontinence. Urgency is a sudden and intense need to pass urine that cannot be put off and urge incontinence refers to the leakage of urine associated with the sensation of urgency. Fascial slings are not meant to cure symptoms of urgency and urge incontinence and these symptoms may worsen in up to 10% of women following a fascial sling procedure.
- Pain. Studies suggest that after a stress incontinence procedure about 1 in 100 women (1%) will develop some pelvic, vaginal, or groin pain. In rare cases the pain may not settle, and removal of the sling is then required.
