Maternal Pelvic Floor Trauma
Pregnancy and childbirth are unique experiences in the life of women. The outcome of a healthy mother and healthy baby are desirable end points, but many factors can influence the outcome of any pregnancy or childbirth. Sometimes childbirth may need to be aided by assisted delivery in the form of cesarean section or operative vaginal delivery with forceps or the ventouse (suction cup).
In this Health Topic
A maternal event is any event that can be directly attributable to pregnancy or childbirth. These events are not limited to the duration of either pregnancy or childbirth and may only become problematic several years after childbirth.
The pelvic floor is composed of a sheet of muscle fibers and connective tissues which span the area underneath the pelvis between the pubic bone at the front and the sacrum (tail bone) at the back (see Figure 1). The pelvic floor supports the uterus, vagina, bladder and rectum. The urethra, vagina and rectum pass through the pelvic floor in an area known as the levator hiatus. This is the weakest area of the pelvic floor. The anal sphincter is a muscle that surrounds the back passage and is often regarded as part of the pelvic floor (see Figure 2).
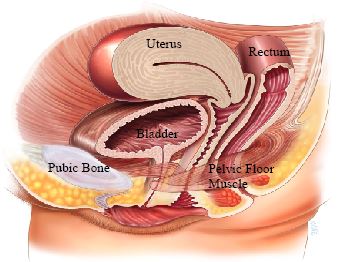
Figure 1
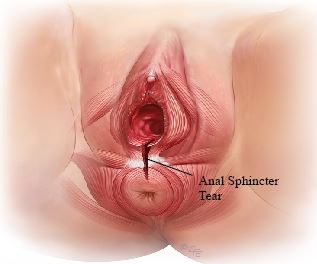
Figure 2- Anal Sphincter
Maternal pelvic floor trauma is when there is damage to the muscles, nerves, or other tissues of the pelvic floor which affects their functioning and leads to weakness of the pelvic floor. Forms of trauma can be divided into:
- Mechanical injury. Injury resulting from the head of the fetus compressing, tearing or forcibly moving the muscle/connective tissues of the pelvic floor. Such injuries may also be caused by the forceps when used to perform an operative vaginal delivery.
- Nerve injury. The pudendal nerve is the main nerve that supplies the pelvic floor. It can be compressed and damaged by the fetal head, a big baby, prolonged second stage of labor, and/or instrumental (particularly forceps) delivery.
- Indirect injury. During pregnancy there are numerous hormonal and physiological changes that take place. These changes include the pelvic floor relaxing at the same time as the load put on the woman’s body increases due to the weight of the baby, the water around the baby, etc. These changes will occur regardless of the final outcome of pregnancy and cannot be avoided
Vaginal delivery (spontaneous or assisted) is the single risk factor most likely to cause maternal pelvic floor trauma. The first delivery tends to be associated with the greatest amount of damage. However, some women can identify the specific pregnancy or delivery that seemed to have the greatest adverse impact on their pelvic floor function.
Common risk factors for maternal pelvic floor damage include:
- Vaginal birth (especially the first vaginal birth)
- Pregnancy
- Advanced maternal age
- Assisted delivery with forceps
- Raised Body Mass Index (BMI)
- Big baby
- Prolonged second stage of labor (i.e. when actively pushing)
- Deep and extensive vaginal wall/perineal/sphincter tears (see Third and Fourth Degree Perineal Tears leaflet)
Women may experience problems during pregnancy, immediately or very shortly after childbirth, or months/years later. Some women will be aware of symptoms for months or years before they mention them or seek help. These can be divided into four main areas:
- Urinary problems. Leaking urine (urinary incontinence), especially when coughing, laughing, sneezing, or exercising (stress urinary incontinence), is the most well recognized urinary symptom of maternal pelvic floor damage. Other symptoms include increased daytime frequency (8 or more times) or increased night-time frequency (more than once).
- Bowel problems. Anal incontinence is a bowel problem resulting from maternal pelvic floor damage (see Fecal Incontinence leaflet). Leakage of gas (flatus incontinence), soiling of underwear (passive leakage), and needing to rush to the toilet to move bowels (fecal urgency) are some of the bowel problems experienced by women. Some women will experience incomplete bowel emptying related to the development of prolapse of the posterior vaginal wall (back wall) or top of the vagina (vault). Methods adopted by women with incomplete emptying include returning to the toilet to try to empty their bowel, pushing with their fingers on the perineum (area between the vagina and anus) or needing to place a finger in the vagina or rectum.
- Sexual problems. During intercourse, pain may be experienced at the entrance to the vagina. This may be due to scar tissue from vaginal tears or cuts made deliberately (episiotomy) to aid childbirth (see Figure 3).
- Symptoms of prolapse. Prolapse is a condition in which one or more of the pelvic organs bulge or herniate into or out of the vagina. Some women first become aware of a prolapse when they feel a lump near the entrance to the vagina (e.g. in the shower). The feeling of a bulge, pressure, heaviness and fullness within the vagina are other common complaints reported by women suffering from pelvic organ prolapse (see Pelvic Organ Prolapse leaflet).
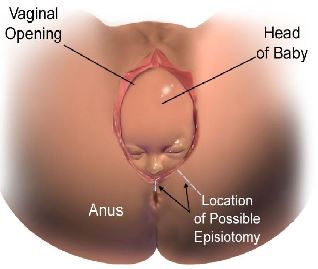
Figure 3- Episotomy
It is important to recognize that some factors cannot be prevented, as they are part of the course of pregnancy. Reducing the risk of pelvic floor trauma is aimed at targeting factors that can be influenced without placing the pregnancy at risk and includes the following:
- Avoiding operative vaginal delivery. This can be achieved by early resort to cesarean section if labor is not progressing properly and is identified in a timely manner. Avoidance is not always possible. Sometimes it is safer to perform an operative vaginal delivery, for example, when the baby’s head is very low and cesarean section would be difficult. Using the ventouse (vacuum) instead of forceps is preferable and less likely to result in tears to the pelvic floor muscle and anal sphincter.
- Delivery by cesarean section. This is very controversial. Evidence suggests that delivery by cesarean section is only protective to the maternal pelvic floor if the woman only has two deliveries. Beyond two deliveries, the protective effective is no longer apparent. Delivery by cesarean section also has risks, which can be significant and increase with the number of cesarean sections.
- Avoiding a prolonged active second stage of labor, i.e. the time from pushing with the cervix being fully open (dilated) to the delivery of the baby. There is a lot of pressure and pushing on the pelvic floor during this period. Hence, labor needs to be actively managed to prevent undue prolongation of this stage of labor.
- Appropriate use of delivery techniques during the final phase of delivery, including cooperation between the mother and attending personnel, control of the fetal head during delivery, manual support and protection of the perineum, and using the correct method to cut and repair episiotomy when needed (see Figure 3) are all important in protecting the pelvic floor.
- Early delivery if the baby is big (for example 4.5kg or more).
- Losing weight before pregnancy to achieve a normal Body Mass Index (BMI) and maintaining normal weight after pregnancy (lifelong).
Treatment of maternal pelvic floor trauma can include conservative and surgical options. Treatment will need to be focused on the specific problems you are experiencing and the findings of your doctor. While there is some overlap, the management of urinary, bowel, sexual, and pelvic organ prolapse problems are different and will be discussed with you by your doctor.
Conservative treatment may include:
- Pelvic floor exercises with a pelvic floor physiotherapist (see Pelvic Floor Exercises leaflet)
- Temporary use of vaginal support pessaries (see Vaginal Pessary for Pelvic Organ Prolapse leaflet)
Surgery will need to be tailored to the individual woman’s circumstances, taking into account:
- The problems you are experiencing
- The findings of your doctor on examination and the outcomes of any investigations
- Whether you consider your family to be complete or not
Direct repair of tears to the pelvic floor muscle is in its infancy and only offered in the context of research studies. Direct repair of anal sphincter muscle tears is commonly performed immediately after childbirth (see Third and Fourth Degree Perineal Tears leaflet), but sometimes this is also done later in life in women with anal incontinence. However, prevention is much more effective than repair.
The general advice is to complete your family prior to surgery. Individual circumstances and the degree of problems you are experiencing may make this not always practicable and even though surgery can be repeated, it is important to get specialist advice about this. If a further pregnancy is contemplated after pelvic floor surgery, it is important to discuss the delivery options with your obstetrician and pelvic floor surgeon.
