Posterior Vaginal Wall & Perineal Body Repair
In this Health Topic
About 1 in 10 women require surgery for vaginal prolapse. A prolapse of the back (posterior) wall of the vagina is usually due to a weakness in the strong tissue layer (fascia) that divides the vagina from the lower part of the bowel (rectum). This weakness may cause difficulty when passing a bowel movement, a feeling of fullness or dragging in the vagina or an uncomfortable bulge that may extend beyond the vaginal opening. Other names for the weakness of the back wall of the vagina include rectocele and enterocele.
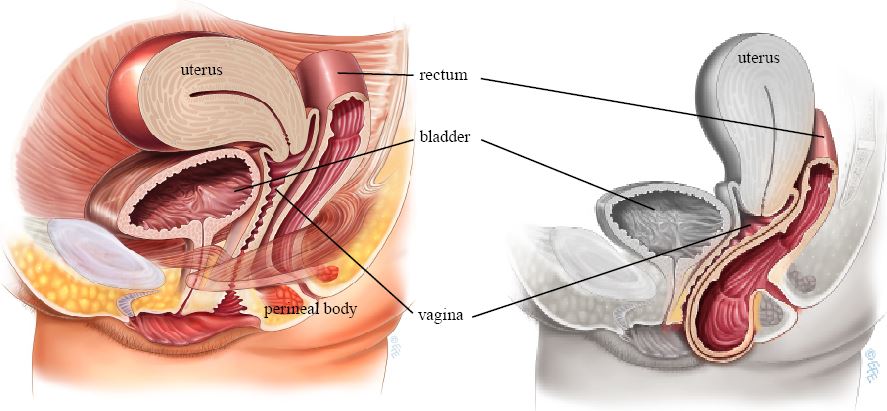
Normal anatomy, no prolapse (left), and Posterior wall prolapse (right)
A posterior repair, also known as a posterior colporrhaphy, is a surgical procedure to repair or reinforce the fascial support layer between the rectum and the vagina. A perineorrhaphy is the term used for the operation that repairs the perineal body. The perineal body (the supporting tissue between vaginal and anal openings) also helps to support the back wall of the vagina. The perineum is the area that is often damaged when tears or episiotomies occur during childbirth. This area may need to be repaired along with the back wall of the vagina to give perineal support and in some cases reduce the vaginal opening.
The aim of surgery is to relieve the symptoms of vaginal bulge and/or laxity and to improve or maintain bowel function without interfering with sexual function.
The surgery can be performed under general, regional or even local anesthetic; your doctor will discuss which is best for you. There are many ways to perform a posterior repair. Below is a general description of a common repair method.
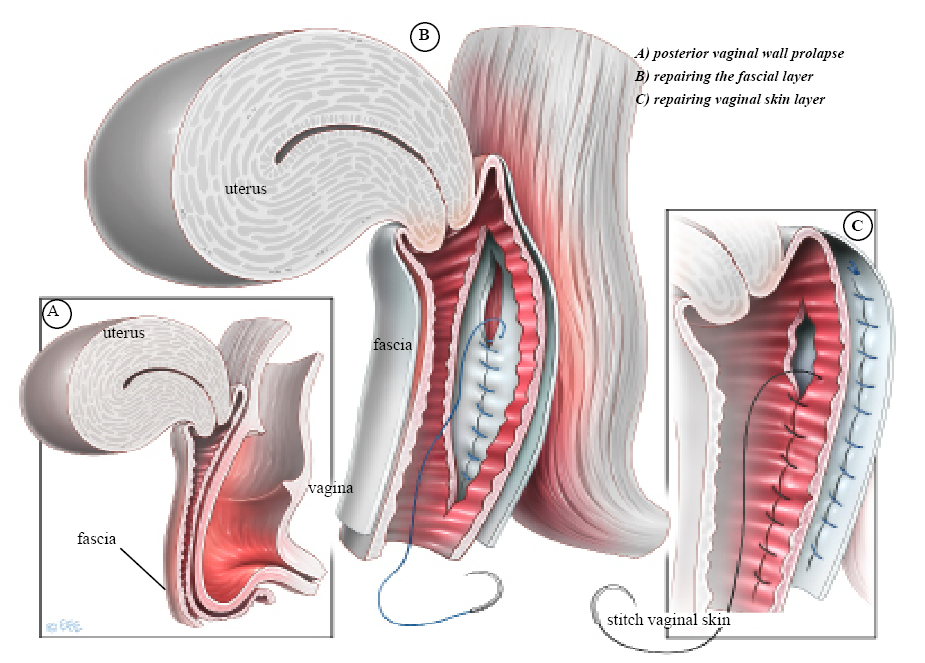
- An incision is made along the center of the back wall of the vagina starting at the entrance and finishing near the top of the vagina.
- The vaginal skin is then separated from the underlying supportive fascial layer. The weakened fascia is then repaired using absorbable stitches. These will absorb over 4 weeks to 5 months depending on the type of stitch (suture) material used.
- The perineal body may then be repaired by placing deep sutures into the underlying perineal muscles to build up the perineal body.
- The overlying skin is then closed with absorbable sutures. These dissolve after 4 to 6 weeks and do not need to be removed.
- A pack may be placed into the vagina and a catheter into the bladder at the end of surgery. If so, this is usually removed after 3 to 48 hours. The pack acts like a compression bandage to reduce vaginal bleeding and bruising after surgery.
- Commonly, posterior vaginal repair surgery may also be combined with other surgery such as vaginal hysterectomy, anterior vaginal wall repair or incontinence surgery.
You will be asked about your general health and medication that you are taking. Any necessary investigations (for example, blood tests, ECG, chest x-ray) will be organized. You will also receive information about your admission, hospital stay, operation, pre- and post-operative care.
When you wake up from the anesthetic you will have a drip to give you fluids and may have a catheter in your bladder. The surgeon may have placed a pack inside the vagina to reduce any bleeding into the tissues. Both the pack and the catheter are usually removed within 24 hours of the operation.
It is normal to get a discharge for 4 to 6 weeks after surgery. This is due to the presence of stitches in the vagina; as the stitches absorb the discharge will gradually reduce. If the discharge has an offensive odor contact your doctor. You may get some blood-stained discharge immediately after surgery or starting about a week after surgery. This blood is usually quite thin and old, brownish looking and is the result of the body breaking down blood trapped under the skin.
Quoted success rates for posterior vaginal wall repair are 80-90%. There is a chance that the prolapse might come back in the future, or another part of the vagina may prolapse.
About 50% of women who have symptoms such as incomplete bowel emptying or constipation will have improvement in their symptoms following surgery.
With any operation there is always a risk of complications. The following general complications can happen after any surgery:
- Anesthetic problems. With modern anesthetics and monitoring equipment, complications due to anesthesia are very rare, but can happen.
- Bleeding. Serious bleeding requiring blood transfusion is unusual following vaginal surgery (less than 1%).
- Post-operative infection. Although antibiotics are often given just before surgery and all attempts are made to keep surgery sterile, there is a small chance of developing an infection in the vagina or pelvis.
- Bladder infections (cystitis). Bladder infections occur in about 6% of women after surgery and are more common if a catheter has been used. Symptoms include burning or stinging when passing urine, urinary frequency and sometimes blood in the urine. Cystitis is usually easily treated by a course of antibiotics.
The following complications are more specifically related to posterior vaginal wall repair:
- Constipation is a common post-operative problem and your doctor may prescribe laxatives for this. Try to maintain a high fiber diet, drink plenty of fluids and use a stool softener. Remember constipation also contributes to forming a posterior wall prolapse and it is therefore important to avoid getting constipated.
- Some women develop pain or discomfort with intercourse. While every effort is made to prevent this from happening, it is sometimes unavoidable. Some women also find intercourse is more comfortable after their prolapse is repaired.
- Damage to the rectum during surgery is a very uncommon complication.
In the early post-operative period, you should avoid situations where excessive pressure is placed on the repair, i.e. lifting, straining, vigorous exercise, coughing and constipation. Maximal strength and healing around the repair occurs at 3 months and care with heavy lifting (>10kg/25lbs) needs to be taken until this time.
Your doctor can guide you as to time taken off from work, as this will depend on your job type and the exact surgery you have had.
You should be able to drive and be fit enough for light activities such as short walks shortly after surgery.
You should wait six weeks before attempting sexual intercourse. Some women find using additional lubricant during intercourse is helpful. Lubricants can easily be bought at supermarkets or pharmacies.