Stress Urinary Incontinence
In this Health Topic
Stress Urinary Incontinence (SUI) is the involuntary leakage of urine during activities such as coughing, sneezing, lifting, laughing or exercising. SUI affects at least 10-20% of women, many of whom do not realize that there are simple, effective treatment options available.
SUI affects the quality of women’s lives in many ways. Incontinence may limit women’s social and personal relationships as well as limit physical activity.
As urine is produced and fills the bladder, the bladder (detrusor) muscle relaxes and stretches to accommodate the fluid. When the bladder is filled to a certain level, an urge to pass urine is felt, and when it is appropriate, the brain signals the detrusor muscle to contract and the urethral sphincter to relax, thus allowing urine to be passed. The bladder usually needs to be emptied about 5-7 times per day, and 1-2 times at night.
The urethra (tube that carries urine out of the body) and bladder are supported by the pelvic floor muscles, which contract during coughing, sneezing and exercise to prevent leakage. Weakness in the muscles or damage to the bladder neck support can result in leakage.
- Pregnancy and vaginal birth
- Obesity, chronic cough, chronic heavy lifting and constipation can cause an increase in abdominal pressure and aggravate stress incontinence
- Genetically inherited factors
Your physician will ask questions about activities which cause leakage and will normally examine you to see if there are any other relevant problems, such as prolapse. Women with stress incontinence may also have problems with urinary urge incontinence, or incontinence of feces or gas. Do not feel embarrassed to mention these problems to your doctor.
- To help with diagnosis, your doctor may ask you to cough while you have a comfortably full bladder.
- You may be asked to fill in a frequency volume chart (bladder diary), recording how much you drink, as well as the number of times you pass urine and the volume passed each time. A record of the amount of leakage is also kept.
- Your doctor may recommend urodynamic studies. Urodynamics investigate the bladder’s ability to fill and empty, and the mechanism or cause of the incontinence.
- An ultrasound scan may be used to determine how much urine is left in the bladder after it empties and can identify if there are any other causes for your symptoms.
- A urine test may be performed to look for a urinary tract infection.
All these tests are designed to help plan the best treatment for each individual.
Your physician will advise you on the best options for you, but initially conservative treatment may be recommended.
- General lifestyle changes. Aim to drink enough to pass urine 4 to 6 times per day (usually about 1.5-2 liters; half a gallon). Maintaining weight within a healthy range has been shown to reduce the severity of SUI problems. Avoiding causes of constipation and cutting out smoking can also help.
- Pelvic floor exercises. Pelvic Floor exercises (PFE) can be a very effective way of improving symptoms of SUI. Up to 75% of women show an improvement in leakage after PFE training. Like all training, the benefits of pelvic floor exercises are maximized if practice is carried out regularly over a period of time. Maximum benefit usually occurs after 3 to 6 months of regular exercising. You may be referred to a therapist who specializes in teaching PFEs to supervise this. If you also have a problem with urge urinary incontinence, your doctor may also advise bladder training exercise.
- Continence devices. Continence devices are available which fit in the vagina and help control leakage. These can be inserted prior to exercise or in the case of a vaginal pessary, worn continuously. Some women find inserting a large tampon prior to exercise may prevent or reduce leakage. These types of devices are most suitable for women with minor degrees of urinary incontinence or who are waiting definitive surgical treatment.
The aim of surgery is to correct weakness of the supports of the bladder neck. Many surgeons would want to avoid surgery until a woman’s family is complete because future pregnancy may compromise the results of the initial surgery.
Mid-urethral sling procedures. Before 1993, the treatment of stress incontinence often involved major surgery with an abdominal incision. The most common treatment now involves the use of a permanent sling that lies under the middle section of the urethra. The sling works by providing support to the urethra when you cough, sneeze or exercise. Following a small incision in the vagina, the sling can be put into position in a number of ways.
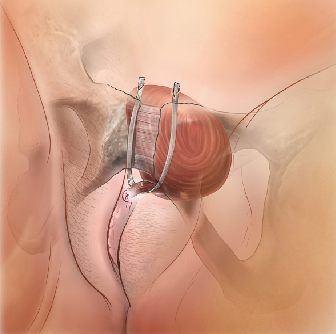
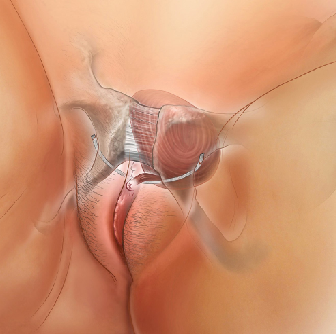
- Retropubic slings pass under the urethra, then run behind the pubic bone with the tape exiting out through two small cuts just above the pubic bone.
- Transobturator slings run under the mid part of the urethra and pass out through 2 incisions in the groin.
- Single incision slings pass under the urethra and are anchored within the tissues. This type of sling has been less well studied to date.
80-90% of women undergoing retropubic or transobturator sling procedures are cured or have improvement of their stress incontinence symptoms following surgery. Single incision sling procedures are fairly new, and success rates are still being monitored.
This operation is not designed to cure urge incontinence/overactive bladder (OAB) symptoms, although up to 50% of women notice some improvement in OAB symptoms following sling surgery. However, in a small percentage of women with OAB, their symptoms may worsen.
Most women will recover from surgery within 2-4 weeks. Some women will have an aching discomfort in the groin for a couple of weeks. A small amount of vaginal bleeding for 7-10 days following surgery is not unusual.
Mesh sling procedures have been done safely for many years, however, in view of the recent media coverage of vaginal meshes, we have provided answers to frequently asked questions about meshes on our website (click here).
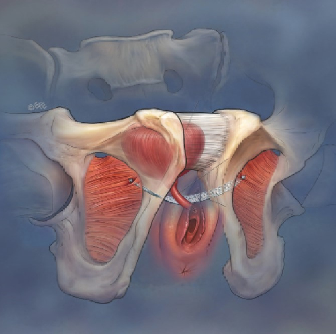
Autologous fascial sling. This type of sling is made out of tissue from the patient´s own body. The fascia is a layer of strong connective tissue usually obtained from the abdomen or thigh. A strip of fascia 1-3cm wide is placed under the urethra to give support and reduce leakage of urine. The operation is done under anesthesia and involves two steps. First, the surgeon will take a strip of the fascia from the abdomen through a cesarean section-like incision, or from the thigh via a small incision. Second, a small cut is made in the vagina, under the urethra. The strip of fascia is secured underneath the urethra and then passed up to the abdominal wall. The small cut in the vagina is then closed. Fascial slings are as successful as synthetic mesh slings with success rate of 80-90%.
Burch (colposuspension). For many years, this was considered the main operation for the management of SUI. It is performed either through a 10-12cm lower abdominal incision (open Burch) or as a laparoscopic (‘key hole’) approach. The surgery involves the passage of 4-6 permanent sutures that suspend the vaginal tissue underlying the bladder to the back of the pubic bone in order to support the bladder neck and urethra and restore continence. Open Burch colposuspension has a success rate similar to that of retropubic slings in long-term follow-up studies, and comparable results can be obtained by skilled surgeons using the laparoscopic approach.
Bulking agents. Substances can be injected around the bladder neck and into the urethral sphincter to bulk it up and reduce the caliber of the urethra. A variety of different substances can be injected including fat and collagen. The injection can be performed in the office or outpatient surgery. An anesthetic may be required for the operation, but many are performed under local anesthetic only. Some burning or stinging when urinating, after the operation, is quite common. Sometimes injections need to be repeated. Complications will vary depending on the type of bulking agent used, and you should discuss these with your doctor.