Sacrospinous Fixation/Illeococcygeus Suspension
Prolapse of the vagina or uterus is a common condition with 11-19% of women undergoing surgery for prolapse during their lifetime. Prolapse often occurs as a result of damage to the support structures of the uterus and vagina.
Symptoms related to prolapse include a bulge or sensation of fullness in the vagina, or an external bulge that extends outside the vagina. It may cause a heavy or dragging sensation in the vagina or lower back and difficulties with passing urine or bowel movements. For some women it causes difficulty or discomfort during intercourse.
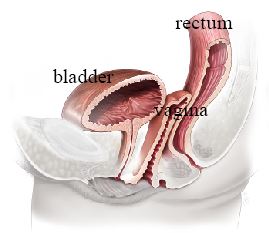
Normal vaginal vault with no prolapse
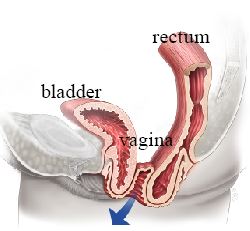
Vaginal vault prolapse, with prolapse of the bladder and rectum
In this Health Topic
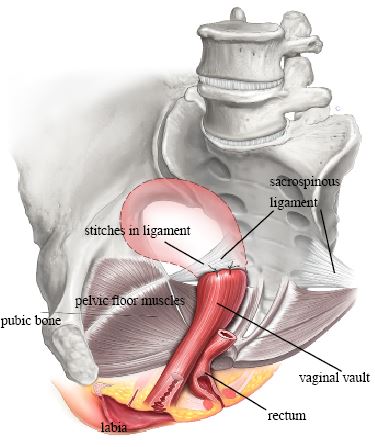
A sacrospinous fixation is an operation designed to restore support to the uterus or vaginal vault (in a woman who has had a hysterectomy). Through a cut in the vagina, stitches are placed into a strong ligament (sacrospinous ligament) in the pelvis and then to the cervix or vaginal vault. The stitches can be either permanent or slowly absorbed over time. Eventually they are replaced by scar tissue that then supports the vagina or uterus. This procedure is often combined with a vaginal hysterectomy and/or surgery to treat prolapse of the bladder, bowel, or stress urinary incontinence.

Sacrospinous fixation with stitches in both sacrospinous ligaments
Sacrospinous fixation stitches into right ligament shown with the uterus present
You will be asked about your general health and medication that you are taking. Any necessary investigations (for example, blood tests, ECG, pelvic ultrasound, chest x-ray) will be organized. You will also receive information about your admission, hospital stay, operation, pre- and post-operative care.
When you wake up from the anesthetic you will have a drip to give you fluids and may have a catheter in your bladder and provided with adequate pain relief. Often the surgeon will place a pack inside the vagina to reduce any bleeding into the tissues. Both the pack and the catheter are usually removed within 24-48 hours of the operation. You will be required to stay for 1-2 days in the hospital.
It is normal to get a creamy white discharge for 4-6 weeks after surgery. This is due to the presence of stitches in the vagina. As the stitches absorb, the discharge will gradually reduce. If the discharge has a bad smell, contact your doctor as treatment with antibiotics may be required.
You may get some blood-stained discharge immediately after surgery or starting about a week after surgery. This blood is usually quite thin and old, brownish looking, and is the result of the body breaking down blood trapped under the skin.
The outcomes, complications and recovery are similar for both Sacrospinous fixation and Ileococcygeal suspension. Quoted success rates for sacrospinous fixation and ileococcygeus suspension are between 80-85%. However, there is a chance that the prolapse might come back in the future, or another part of the vagina may prolapse for which you would need further surgery.
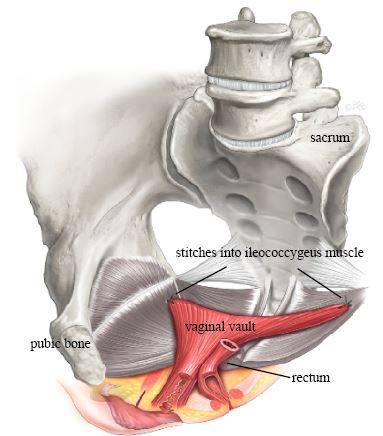
Ileococcygeus Suspension
With any operation there is always a risk of complications. The following general complications can happen after any surgery:
- Anesthetic problems. With modern anesthetics and monitoring equipment, complications due to anesthesia are very rare. Surgery can be performed using a spinal or general anesthetic. Your anesthetist will discuss what will be most suitable for you.
- Serious bleeding requiring blood transfusion is unusual following vaginal surgery.
- Post-operative infection. Although antibiotics are often given just before surgery and all attempts are made to keep surgery sterile, there is a small chance of developing an infection in the vagina or pelvis. Symptoms include an unpleasant smelling vaginal discharge, fever, and pelvic pain or abdominal discomfort. If you become unwell contact your doctor.
- Bladder infection (cystitis). Bladder infections occur in about 6% of women after surgery and are more common if a catheter has been used. Symptoms include burning or stinging when passing urine, urinary frequency, and sometimes blood in the urine. Cystitis is usually easily treated by a course of antibiotics.
The following complications are more specific to sacrospinous fixation/ileococcygeus suspension:
- Approximately 1 in 10 women who have a sacrospinous fixation will get pain in their buttock for the first few weeks after surgery. This will get better by itself and you will be given pain killers to help. It is also quite common to get some stabbing or burning rectal pain that settles within a short time.
- Constipation is a common short-term problem and your doctor may prescribe laxatives for this. Try to maintain a high fiber diet and drink plenty of fluids to help as well.
- Some women develop pain or discomfort with intercourse. While every effort is made to prevent this from happening, it is sometimes unavoidable. Some women also find intercourse more comfortable after their prolapse is repaired.
- In rare cases, bladder and bowel damage to the ureter (the tube conducting urine from the kidney to the bladder) may occur and require surgical repair.
- Stress urinary incontinence can develop in 1 in 3 women with urine leakage on coughing, laughing or sneezing. This is because correction of prolapse results in unkinking of the urethra which may be inherently weak but was masked by the prolapse. The possibility of developing leakage can be tested prior to surgery by bladder tests and additional surgery considered after discussion with your specialist.
- Bladder emptying generally improves in majority but 1 in 10 can continue to have difficulty with emptying or voiding dysfunction.
You should be able to drive and be fit enough for light activities such as short walks within a month of surgery. We advise you to avoid heavy lifting and sports for at least 6 weeks to allow the wounds to heal. It is usually advisable to plan to take 4-6 weeks off work. Your doctor can guide you as this will depend on your job type and the exact surgery you have had.
You should wait six weeks before attempting sexual intercourse. Some women find using additional lubricant during intercourse is helpful. Lubricants can easily be bought at supermarkets or pharmacies.
