Sacrocolpopexy
Introduction
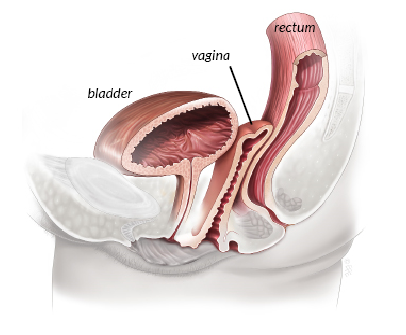
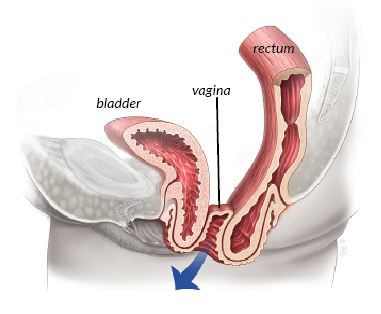
Vaginal prolapse is a common condition causing symptoms such as a sensation of bulging, fullness or pressure in the vagina; difficulty emptying the bowel or bladder, and backache. About 1 in 10 women need surgery for prolapse of the uterus or vagina. Vault prolapse is when the upper vaginal support weakens, resulting in the vagina dropping “downward” towards the entrance (see illustration).
In this Health Topic
Sacrocolpopexy is a procedure to correct prolapse of the vaginal vault (top of the vagina) in women who have had their uterus removed (hysterectomy). The operation is designed to restore the vagina to its normal position and function. A variation of this surgery called sacrohysteropexy (in women wishing to preserve their uterus) is performed in a similar way to sacrocolpopexy.
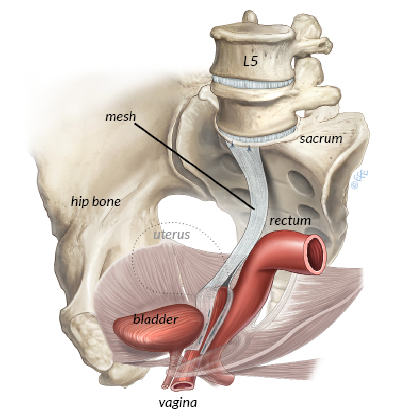
Sacrocolpopexy is performed either through an abdominal incision or “key holes” (using a laparoscope or with a surgical robot). Surgery is done under general anesthesia, which is means being completely asleep with a tube in your throat to breathe. The vagina is first freed from the bladder at the front, and from the rectum at the back. A graft made of permanent synthetic mesh (lightweight material made from woven polypropylene) is used to cover the front and the back surfaces of the vagina. The mesh is then attached to a ligament that runs on the sacrum (tail bone) as shown in the illustration. The mesh is then covered by a layer of tissue called the peritoneum that lines the abdominal cavity. This prevents the bowel from getting stuck to the mesh. Please note that the abdominal mesh is not included in the recent controversies involving vaginal meshes (see our FAQ section on www.yourpelvicfloor.org). Sacrocolpopexy can be performed at the same time as surgery for urinary incontinence or vaginal wall repairs.
Studies show that 80-90% of women having sacrocolpopexy are cured of their prolapse and prolapse symptoms. Following surgery there is a small risk of prolapse developing in another part of the vagina, such as the front wall that supports the bladder. If this does develop, it may require further surgery.
The most commonly reported complications for both open and laparoscopic techniques include:
- Pain (generally or during intercourse) in 2-5%
- Mesh exposure / erosion in 2-4% of cases. There is a small risk of mesh erosion into the surrounding organs such as bladder, bowel or vagina. This is uncommon but may require a repeat operation to trim the mesh or remove the mesh.
- Damage to the bladder, bowel, or ureters in 1-2%
- Changes in bowel movement (constipation, slow bowel, bowel obstruction) in 2-3%
- Changes in urination – up to 10% of women may have trouble emptying their bladder or have slower urine stream immediately after surgery. This usually resolves on its own within the first few weeks after surgery.
There are also general risks associated with surgery that include wound infection, urinary tract infection, bleeding requiring a blood transfusion, and deep vein thrombosis (clots) in the legs, chest infection, and heart problems. Your surgeon or anesthetist will discuss any additional risks that may be relevant to you.
Medications like aspirin taken regularly affect the clotting system and may need to be stopped before surgery. Some surgeons recommend bowel preparation prior to surgery and your doctor will instruct you if this is required. In most cases you will be asked to avoid food and fluid for 6 hours before surgery.
You will wake up with a catheter in your bladder. The surgeon may have placed a pack inside the vagina to reduce any bleeding into the tissues. You may go home the same day or require a hospital stay for observation. During the first 6 weeks you may be asked to avoid strenuous housework or lifting, including shopping bags, laundry baskets, etc.
Gentle walking is good exercise. Start with about 10 minutes a day when you feel ready and build up gradually. Avoid any fitness-type training, aerobics, etc. for at least 6 weeks after surgery. Swimming, spa baths and intercourse should also be avoided for 6 weeks following surgery. Generally, you will need 4-6 weeks off work. This period may be longer if you have a very physical job.