Uterosacral Ligament Suspension
Prolapse of the vagina or uterus is a common condition with up to 11% of women requiring surgery during their lifetime. Prolapse generally occurs because of damage to the support tissues of the uterus and vagina; this is common following childbirth, from straining with constipation and after menopause. The top of the vagina can still prolapse following a hysterectomy, this is called vault prolapse (vault-top of the vagina in a woman who has had a hysterectomy).
Symptoms related to prolapse include a bulge or sensation of fullness in the vagina, or an uncomfortable bulge that extends outside of the entrance to the vagina. It may cause a heavy or dragging sensation in the vagina or lower back and difficulties with passing urine or bowel motions. For some women it causes difficulty or discomfort during intercourse.
In this Health Topic
A uterosacral ligament suspension is an operation designed to restore support to the uterus (womb) or vaginal vault.
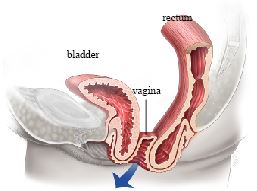
Vaginal Vault Prolapse
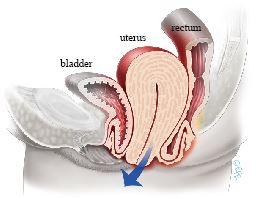
Uterine Prolapse
The uterosacral ligaments are strong supportive structures that attach the cervix (neck of the womb) to the sacrum (bottom of the spine). Weakness and stretching of these ligaments can contribute to pelvic organ prolapse.
A uterosacral ligament suspension involves stitching the uterosacral ligaments to the apex or top of the vagina, thereby restoring normal support to the top of the vagina. This operation can be done vaginally, abdominally or laparoscopically (“keyhole”), and your surgeon will discuss these options with you. It is also sometimes done at the time of a hysterectomy in order to reduce the risk of prolapse in the future and can be combined with other procedures for prolapse or incontinence. Either absorbable (dissolvable) sutures (stiches), or non-absorbable (permanent, non-dissolving) sutures can be used, speak to your surgeon about which one will be used. Sutures can be placed on one side, or both sides, depending on surgeon preference.
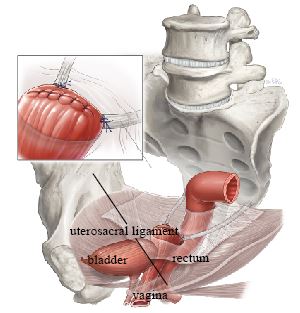
Uterosacral Ligament Suspension
You will be asked about your general health, previous surgery and any medication that you are taking. Any necessary investigations (for example, blood tests, ECG, chest x-ray) will be organized. You will also receive information about your admission, hospital stay, operation, pre- and post-operative care.
When you wake up from the anesthetic you will have a drip (IV) to give you fluids and may have a catheter in your bladder. Often the surgeon will place a pack (a wad of gauze material) inside the vagina to reduce any bleeding into the tissues. Both the pack and the catheter are usually removed within 24-48 hours of the operation. It is normal to get a creamy white or yellow discharge for 4-6 weeks after surgery. This is due to the presence of stitches in the vagina; as the stitches absorb, the discharge will gradually reduce. If the discharge has a bad odor, contact your doctor. You may get some blood-stained discharge immediately after surgery or starting about a week after surgery.
Quoted success rates for uterosacral ligament suspension are between 80 to 90%. However, as with any prolapse surgery, there is a chance that the prolapse might come back in the future, or another part of the vagina may prolapse, for which you would need further surgery.
With any operation there is always a risk of complications. The following general complications can happen after any surgery:
- Anesthetic problems. With modern anesthetics and monitoring equipment, complications due to anesthesia are very rare. Surgery can be performed using a spinal or general anesthetic. Your anesthetist will discuss what will be most suitable for you.
- Post-operative infection. Although antibiotics are often given just before surgery and all attempts are made to keep surgery sterile, there is a small chance of developing an infection in the vagina or pelvis. Symptoms include an unpleasant smelling vaginal discharge, fever, and pelvic pain or abdominal discomfort. If you become unwell, contact your doctor.
- Bladder infections (cystitis). The chances of developing bladder infections after surgery can range from 7% to 34% and are more common if a catheter has been used. Symptoms include burning or stinging when passing urine, urinary frequency and sometimes blood in the urine. Cystitis is usually easily treated by a course of antibiotics.
- Clots. Clots in the blood vessels of the legs or lungs can be a problem in patients undergoing this type of surgery. You will be given compression stockings to reduce the risk of this, and possibly also a course of blood thinning injections.
Specific complications related to uterosacral ligament suspension include:
- Ureteric injury. Ureteric injury is quoted to occur in 1-10% of women undergoing this procedure (the ureters are the tubes that connect the kidneys to the bladder). At the time of the procedure, your surgeon may look inside the bladder with a telescope (cystoscopy) to check that the ureters are still functioning. Ureteric injury may require further procedures in the future.
- Buttock pain. This is usually a short-term problem that can be managed with pain medication.
- Constipation. This is a common short-term problem. Your doctor may prescribe laxatives for this. Try to maintain a high fiber diet and drink plenty of fluids to help as well.
- Pain with intercourse. This can rarely occur due to scar tissue at the top of the vagina, although most women find that their sex life improves once a prolapse is treated.
You should be able to drive and be fit enough for light activities such as short walks within a month of surgery. We advise you to avoid heavy lifting and sport for at least 6 weeks to allow the wounds to heal. It is usually advisable to take 4-6 weeks off work. Your doctor can guide you as this will depend on your job type and the exact surgery you have had.
You should wait six weeks before attempting sexual intercourse. Some women find using additional lubricant during intercourse is helpful. Lubricants can easily be bought at supermarkets or pharmacies. Your doctor may suggest a course of vaginal oestrogen cream or pessaries.
