Labiaplasty
In this Health Topic
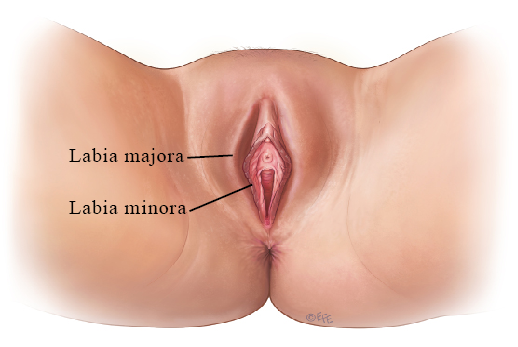
Labiaplasty is a surgery performed to enhance the appearance of the labia or to reconstruct the labia. Alternative names for labiaplasty include:
- Labioplasty
- Labia minora reduction/Nymphoplasty
- Labia majora reduction/Labia majoraplasty
- Labial reduction
Labiaplasty is a controversial subject, but the number of procedures is increasing – perhaps as a result of the availability of information through social media, an increase in genital waxing, or desire to improve one’s self-image and confidence. Some of the reasons stated for performing labiaplasty include:
- Functional issues
- Esthetic (such as asymmetry with one of the labia larger than the other)
- Psychosocial
- Congenital anomalies
- Sex change surgery
The most common functional problem reported is labial discomfort or irritation, usually in association with wearing tight clothing or occurring during activities such as sports and sexual intercourse and splitting/splaying the urine stream. While there is a wide range of anatomical variance in ‘normal’ labial appearance, many women have the perception that their labia are unattractive or have become unattractive. Physical changes can take place at any time and are often gradual, but puberty and pregnancy are events that can be associated with a more rapid, noticeable physical change of the labia. Changes also occur after menopause (including thinning of the lips) or with some vulva conditions. Psychosocial reasons include improvement of sexual life, sexual sensation, self-confidence, quality of life as well as to reduce the signs of vulvo-vaginal aging.
Patients who have congenital conditions such as intersex (a variety of conditions in which a person is born with sexual anatomy or genitalia that doesn’t seem to fit the typical definitions of female or male) or patients undergoing the second stage of male to female gender reassignment may seek to have the labia created where there were none previously.
Any situation related to increased male sex hormone production (such as testosterone) may lead to an undesirable enlargement of the labia minora. This should be ruled out by checking blood hormone levels when suspected.
Labiaplasty may be performed either in the doctor’s office, a day surgery unit, or within a hospital. The setting where the procedure is performed is influenced by the preferences of the surgeon, the complexity of surgery, and the nature of anesthetic used (local anesthesia alone or combined with either a general, regional anesthetic or sedation). Labiaplasty should always be performed by a specialist such as a gynecologist, urogynecologist, or plastic surgeon.
It is desirable for young girls to have had their period for at least two years before performing a labiaplasty. However, sometimes the surgery cannot wait because the size of the labial lips is too excessive and causes self-esteem and functional problems.
Numerous techniques have been described for achieving reduction of the labia minora. The technique performed will depend on the experience of the surgeon and will be influenced by the desired end result. The instruments used for tissue reduction include both cutting tools and laser technology. The main surgical techniques used include:
Direct excision (surgical removal)
- The original and most common technique, also known as amputation/contouring/edge resection
- Has a high patient satisfaction rate with comparatively low complication rate
- Facilitates removal of hyperpigmented (darkened) edges
- Results in loss of natural, irregular labial edges with a more smooth, cosmetic appearance
Wedge excision
- The resection (removal) can be ‘central’ or ‘inferior’
- Preserves the natural, irregular labial edges
- Allows for the choice of a full-thickness or partial-thickness resection
- A Z-shaped incision can be used to reduce the bulky scar otherwise typical of this technique
- A higher, more extensive incision can be used to reduce prominent tissue next to or immediately above the clitoris
- A possible complication of this technique is the wound rupturing along the incision
De-epithelialization
- An uncommonly used technique
- Can reduce the vertical length of the labia but usually at the expense of increasing the diameter
- Preserves the natural, irregular labial edges
Clitoral unhooding (hoodectomy)
- Used in cases where there is prominent tissue next to or immediately above the clitoris associated with irritation, interference with access to the clitoris, or to improve esthetics
- Can be performed at the same time of labiaplasty or as a separate procedure
- Is often a more complex surgery than labiaplasty, but often performed in conjunction with labiaplasty to achieve a perfect esthetic result
As with any surgical procedure, complications can sometimes occur. Possible complications of labiaplasty include:
- Bleeding
- Infection
- Damage to the labia or clitoris
- Under-correction (not enough tissue excised) or over-correction (too much tissue excised)
- Scar tissue and/or poor wound healing
- Clitoral nerve or labial nerve damage
- Tissue hypersensitivity
- Painful intercourse
- Unsatisfactory or uneven appearance
Before having surgery, you will have an examination and meet with your surgeon to discuss the issues of concern to you, the options available to you, and the risks and benefits of those options. Your surgeon will:
- Need to be satisfied that you have realistic expectations about the outcome of surgery
- Need to give you time between the consultation and procedure to absorb and consider the information
- Decide if a consultation with another doctor, or additional psychological assessment, is appropriate
- Advise you about any conditions that need to be met before you can proceed with the procedure
- Obtain your permission to take pre- and post-procedure photographs. Please note the practice/provision of taking photographs or not will vary from country to country
It is typical to have soreness, bruising and swelling for up to two weeks after labiaplasty. Urinating and sitting during this period may be uncomfortable. Applying ice packs and taking painkillers can help with pain and discomfort. Your doctor or the nurse will explain how to care for the wound while it is healing. Wound care includes:
- Normal genital cleansing with mild, non-abrasive agents like baby shampoo
- Dabbing instead of rubbing the wound
- Avoiding wearing tight underwear and clothing
Your surgeon may prescribe a topical antiseptic cream or oral antibiotics to prevent infection while the wound is healing. Generally following labiaplasty you should:
- Avoid strenuous activities for 3-4 weeks
- Avoid sexual intercourse for 4-6 weeks
- Use sanitary towels instead of tampons for the first few menstrual periods; it can take a couple of months for the skin to fully heal
- Be able to return to normal activities after 2-3 weeks
Notify your surgeon of any concerns you have after surgery.
It is worth mentioning that there are other esthetic procedures on the lips, mainly older ones such as filling with fat or hyaluronic acid and laser or radiofrequency application to correct excess wrinkles.